Cataract Surgery & Iris Fixation IOL Technique
In the absence of capsular support, the ophthalmic surgeon is faced with a number of choices for implantation of an intraocular lens (IOL). Myriad techniques have been described for fixation of an IOL either to the iris or the sclera in the ciliary sulcus.
When faced with a preoperative assessment for IOL placement in cases of zonular weakness or iatrogenic capsular rupture, the ophthalmic surgeon should first do a careful slit-lamp examination looking for adequate anterior capsular support to place an IOL in the ciliary sulcus.
This is likely the least complex of all techniques and is the simplest to perform. If slit-lamp examination is inconclusive, intraoperative examination of the anterior capsule, either from direct visualization with the microscope and pupil enlargement with a secondary instrument or by endoillumination from a pars plana approach, should be attempted.
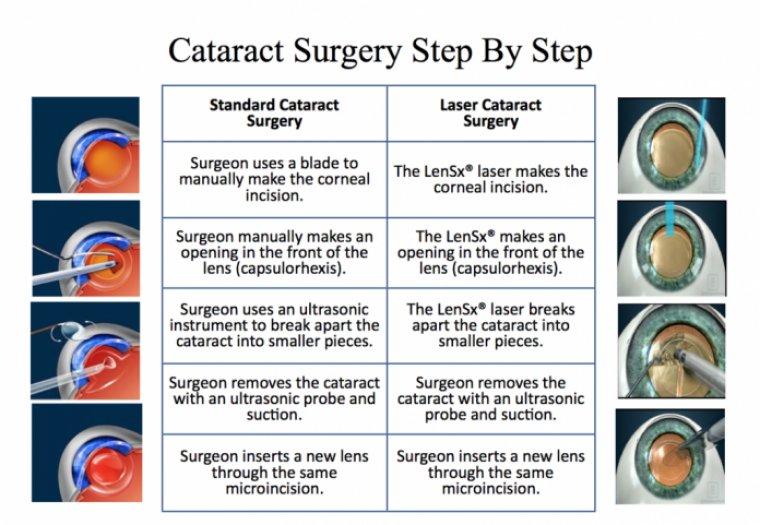
Implantation of intraocular lens has become the standard of care for correction of aphakia after cataract surgery. The development of safe and effective IOL s is one of the great successes in ophthalmology.
Modern PCIOL’s have a track of remarkable safety and provide excellent visual outcome after uncomplicated cataract surgery. Ideally, we aim for IOL placement in the capsular bag which affords stable fixation at a position closer to the nodal point.
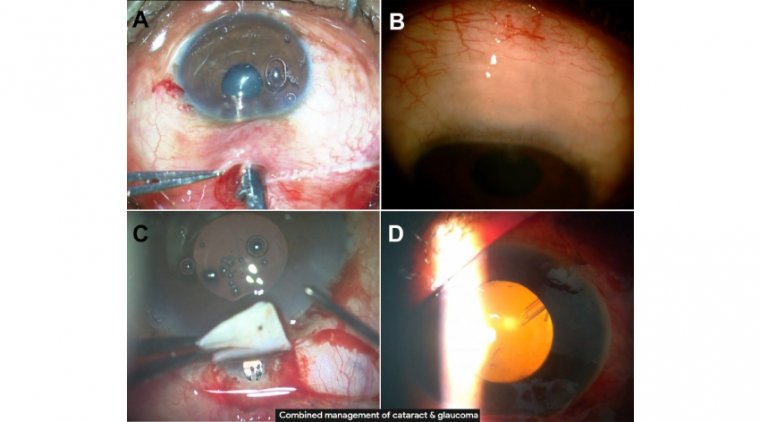
However, in-the bag placement of the IOL is not possible in instances like – congenital zonular weakness, traumatic subluxation or a surgical complication.
In such instances we are left with options of ACIOL, Iris claw lenses and sutured PCIOL s either to sclera or Iris .However, there is no consensus on optimal choice of lens or method and site of fixation, each having its own advantage and disadvantages.
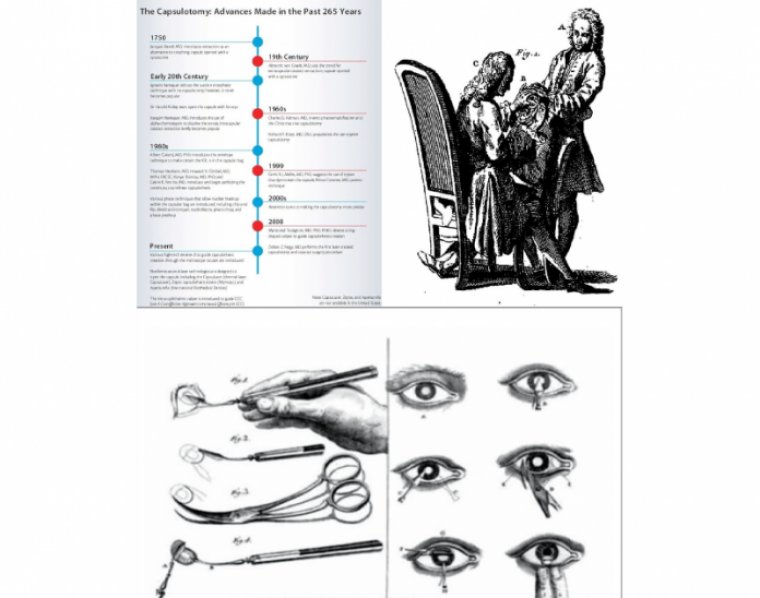
Fixation of the IOL to the iris has become a well –established technique for stabilizing posterior chamber lenses in the lack of adequate capsular support .Its a time tested age old technique first described by Dr McCannel in 1976.
Pre-requisite for Iris fixation IOL is healthy iris tissue with a pupil size of 5mm.
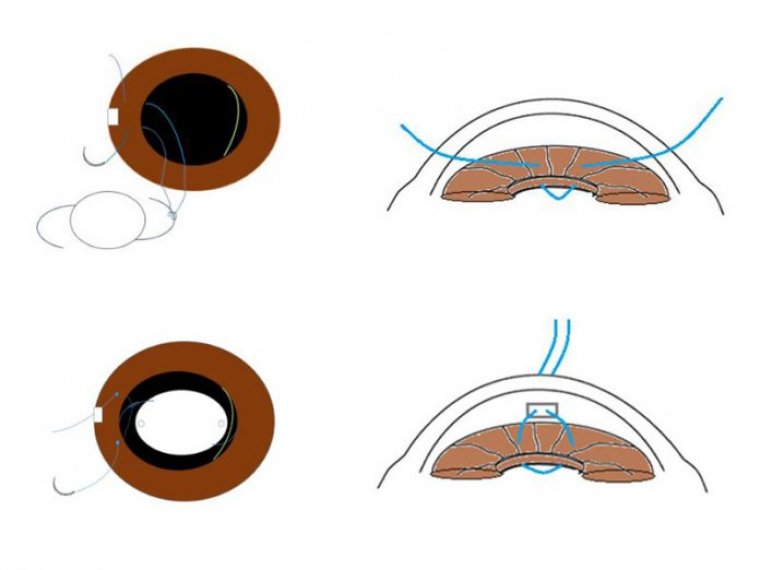
This technique can be performed in two ways.
In the presence of partial capsular bag support, a single haptic fixation of the IOL to the iris can be performed keeping the other haptic rested over the bag remnants or sulcus.It is a safer, time saving procedure with lesser postoperative inflammation and guaranteed IOL stability.
In situations with total loss of capsular bag support, both the haptics of the IOL are sutured to the iris. Literature shows double haptic iris fixation of PCIOL is associated with low risk for IOL drop and postoperative corneal edema.
They have reduced risk of corneal endothelial damage and secondary glaucoma when compared to ACIOL.
Iris fixation of IOLs has proven to have reduced risk for suture exposure and suture breakage compared with the scleral suture technique as the suture is secured well intraocularly.Iris-claw lenses reported a disenclavation rate of 8.7% which can be avoided with iris suture fixation technique.
Post –operative inflammation and CME are relatively less and it does not have any effect on the pupil movement in reaction to light.
Therefore a precise knowledge of the proper technique of secondary Iris fixation techniques mandates reliable and consistent post-operative results in the hands of the novice as well as experienced surgeons.