The Future of Cataract Surgery
Cataract surgery is a modern-day miracle. Since 1995, more than 500 million cataract procedures have been performed worldwide, and about 130 million living people are benefiting from this miracle procedure today.
At present, approximately 35 million cataract procedures are performed every year worldwide. About 70,000 cataract procedures are performed every day globally.
Many people develop cataracts in addition to presbyopia as we age. A cataract is a clouding of the eye’s natural crystalline lens, creating blurriness that cannot be corrected with glasses or contact lenses.
The mean age of the patient undergoing cataract surgery will decline 5 years, from 73 today to 68 in 2030. The cataracts removed will be softer or softened by FLACS, other devices or medications, and phaco aspiration will replace phacoemulsification for most cases, making surgery safer and faster.
A significant number of surgeons still use corneal or limbal relaxing incisions generated by a blade or femtosecond laser to treat astigmatism, often in combination with cataract surgery.
Femtosecond laser application to the corneal stroma, which can change the cornea’s refractive index, is being evaluated by several companies.
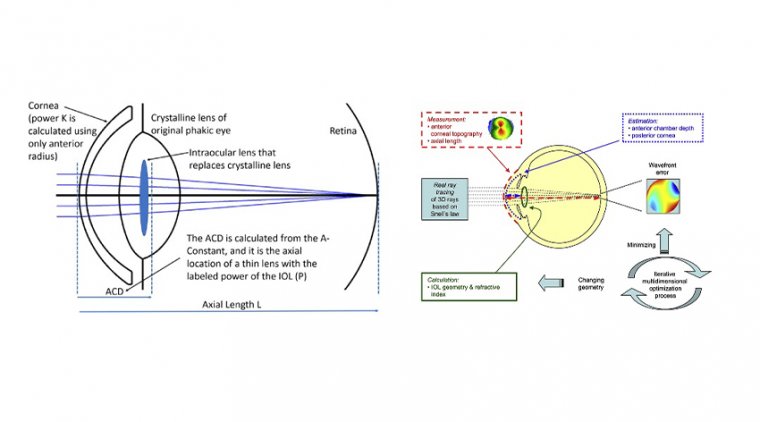
Cataracts are removed surgically and replaced with an artificial intraocular lens (IOL). Monofocal IOLs can address either distance- or near-vision only and patients must still wear glasses.
Multifocal IOLs are very beneficial for presbyopic cataract patients who are motivated to reduce their dependence on wearing bifocals, trifocals, or reading glasses after cataract surgery.
Multifocal IOLs can allow a patient to see both distant and near objects without depending on glasses or contact lenses.
One of the most important and challenging decisions that surgeons face is choosing the right implant technology for each patient when correcting presbyopia and attempting to deliver a spectacle-free refractive solution at the time of cataract surgery.
There is no silver bullet, and there is no substitute for the surgeon’s sitting down one on one with each patient and coming to the most practical and intelligent decision possible based on the patient’s past ocular history, examination, and lifestyle preferences.
Richard L. Lindstrom, MD, is considered to be one of the visionaries in the field of cataract and refractive surgery. He is a pillar in both the practice of ophthalmology and industry of ophthalmology.
Recently, we sat down with Dr. Lindstrom to discuss presbyopia correction, femtosecond laser technology, increasing demand, reimbursement and more.
Kendall E. Donaldson, MD, MS: During the last 10-15 years, so much effort has been placed on overcoming presbyopia. We’ve seen a steady increase in new IOL technology with extended depth of focus IOLs, low-add multifocals, trifocals outside the U.S. (and soon to be here) and adjustable IOL technology in the pipeline. What do you believe is the future of presbyopia correction?
Richard L. Lindstrom, MD: I believe technology will continue to improve and surgeons will become more confident that they can generate an outcome that will make patients happy.
We project growth, and, as a treatment for cataract, I believe that we’ll be able to get presbyopia correction into 25% or so of cataract surgeries as technology improves and as surgeons become more comfortable with the available options for presbyopia correction.
We also think that as technology moves into the era of a truly accommodating IOL that can accommodate 3D or more, we’ll see a growth in clear lens extraction, also known as stage 1 dysfunctional lens syndrome (those patients suffering from very early symptoms of presbyopia).
So we see growth both for the treatment of cataract and for the treatment of natural presbyopia prior to the development of a Snellen visual acuity meaningful cataract.
KD: The market penetration of presbyopic IOLs is only around 8% right now in the United States. Do you attribute this entirely to lack of confidence in the technology?
RL: I think it’s multifactorial. Everyone’s been trying to figure out what’s the golden key. I think the golden key is just continuous, incremental improvement in technology, surgeon training and comfort so that we can start to hit refractive targets required on the first try in a high majority of patients.
The adjustable IOL will make enhancements easier. Only 20% to 25% of us are comfortable doing enhancements with corneal refractive surgery if we miss the target. So that’s certainly a barrier for many surgeons.
But there is a group of patients who are OK wearing glasses. There is a group of patients who find the extra cost excessive, so I think cost will always limit the market penetration.
I believe that if there were no additional fee and if presbyopia correction were reimbursed by insurance carriers, we probably would see most patients selecting presbyopia-correcting IOLs.
I think we will get a 20% to 25% increase in market penetration over the next decade and new technologies will keep coming, and I think that surgeons will get more and more comfortable.
KD: I think when we have the true answer for presbyopia, all of us will have surgery when we’re 40 years old and presbyopia eventually will no longer exist. How far do you think we are from eliminating presbyopia?
RL: I think in 10 years we will have an IOL that accommodates 3D or more, which will make most patients happy. I believe that the implant will also be adjustable without having to do corneal refractive surgery.
So we’ll be able to hit our desired target within 0.25 D every time, ultimately increasing patient satisfaction. So then you’ll see more patients opting for premium lenses, because they’ll be more confident that they can generate the outcome they need to have a happy patient.
KD: We recently celebrated the 50-year anniversary of phaco technology, attributed to Dr. Charles Kelman. Do you think phaco technology will remain the standard of cataract surgery? Do you think some other type of technology will replace phaco?
RL: I believe the major transition that we’re really in the process of is a transition from phacoemulsification to phacoaspiration. Patients are coming in earlier and younger for their cataract surgery, so most of the time we can do phacoaspiration on softer lenses even today.
I think we’ll move towards phacoaspiration, so there will be no issues with heat, therefore we won’t be generating inflammation and free radicals.
We’re probably going to be less likely to break capsules and manage the endothelium better without the occasional chatter and burst of nuclear material that we spread around when we do phacoemulsification. So, I think the big trend will be toward small-incision cataract surgery.
Also, technology companies are working on device technology that would be less expensive, maybe even disposable. I can imagine the day when the tubing and handpiece are all disposable. You still will need a base module, but if it doesn’t have ultrasound it probably will be less expensive.
Also, I think phacoemulsification as we have known it the last 50 years in the U.S. is going to start to penetrate in developing nations.
There are about 26-28 million cataract surgeries a year done outside the U.S., but a relatively small number (less than half) are done with phacoemulsification; probably 6 million are performed with a form of extracapsular cataract surgery.
But surgeons around the world are having the same experience that we are and are starting to see patients earlier in their cataractogenesis.
KD: With a surplus of pre-op technology — femtosecond lasers, intraoperative aberrometry, lasers and lights that may eventually modify IOLs post-operatively — the cost of cataract surgery seems like it will continue to grow.
What do you think we should do to make costs manageable? What can the average cataract surgeon do in a typical private practice to provide the best refractive results for patients but still contain costs?
RL: For the individual surgeon, I would say it’s a small, incremental, year-by-year change. Since I’ve been in ophthalmology, 45 years when I was first trained at the University of Minnesota Hospital, I was trained in intracapsular cataract extraction.
We rarely placed an IOL. We scheduled four cases a day, which meant two hours a case, and the third-party reimbursement was in the $3,000 to 4,000 range to the hospital and close to $3,000 to the surgeon.
We were doing 250,000 to 300,000 cataracts a year in the U.S. at that time. If we were trying to do that today with 4 million cataracts, it would be absolutely impossible.
When I think about what drives this as I look at it around the world, it’s third-party reimbursement. Patient reimbursement for surgery makes a huge difference in what it costs to have the surgery and how the surgery is delivered.
I believe we will have a moment when our world gets turned upside down in the U.S. Using you as an example, Miami County will say, “At Bascom Palmer we have 10,000 cataracts for you to do, and we’re going to give you this much money, and you can do it anyway you want.”
So what are we going to do? We’re going to do bilateral, same-day, sequential cataract surgery. We’ll probably move out of the hospital or ASC or rename the ASC an office-based surgery center so we can reduce the regulatory cost.
There will be a lot more time spent trying to figure out how to do every step of the operation at lower cost when that happens because surgeons will be paying for the costs rather than transferring the costs to a third-party payer through a facility fee that we will have already paid.
Every dollar we spend will be ours, and every dollar not spent will be ours to take home. However, we will need to continue to balance bill for premium services, as we do today. So, if a patient wants to upgrade from the basic surgery, we’ll be able to upcharge for it.
Those upcharges will become even more critically important to us. I think we’re pretty blessed in ophthalmology that we’ve already got upcharges available for the correction of refractive error, and I think that in the future this will include adjustable IOLs and other advanced technology.
We might be able to pay all of our expenses with the base reimbursement, and what we might be taking home will be the upcharges for the premium channel.
KD: You mentioned bilateral, same-day, cataract surgery — like the Kaiser Permanente model. Right now, we are limited with liability issues, finances and logistical issues, but how far do you think we are from actually having that become the primary means by which we do cataract surgery in the United States?
RL: As I said, I think it’s going to be driven by reimbursement. If you were reimbursed the way Kaiser is reimbursed where they have a bucket of money and then they have a bucket of patients to take care of, you have no choice.
So when the day comes when you and I have a bucket of money and a bucket of patients to take care of, we’ll adopt it. But, the way it is now, if you do both eyes in the same day, your reimbursement goes down for the second eye and you’re strongly incented not to do it that way.
Patients will accept it immediately. We can probably learn to do it without any additional risk. Of course, if you have a problem in the first eye, you wouldn’t proceed with the second eye, just like we do when we do LASIK or any other bilateral plastics procedures. But most of the time the case goes smoothly.
In my opinion, that’s definitely going to happen in the next decade. At Kaiser, they’re doing bilateral, same-day, sequential surgery, and interestingly enough, also in several VA hospitals.
KD: With the increasing number of older Americans and patients having cataract surgery at a younger age, the number of cataracts that we’re doing each year has been increasing.
How are we going to serve all of these patients? Do you think telemedicine tools or physician extenders (such as a physician assistant [PA] or an optometrist) might play more of a lead role in delivery of care?
RL: Well, we have an issue — the incidence of cataract is growing at a rate of 3% per year, while I think there’s probably about 50 to 100 more ophthalmologists retiring every year than we’re training.
Some would argue as the makeup of those surgeons changes, they are working somewhat fewer hours. They’re going to have twice as many cataract surgeries to do.
I personally want those cataract surgeries done by a surgeon. When I have my cataract surgery, I want it done by an experienced, fully trained, cataract surgeon.
Outside of specific steps like making and closing incisions, I don’t think that we’ll end up delegating cataract surgery to any other party, whether it be a PA or optometrist or other form of physician extender.
I think there are certain other things though, that we may have to delegate as we surgeons have to spend more and more time in the OR. I can imagine the day when some type of care provider might be able to do some of our laser treatments, more of the postoperative care and preoperative care.
As far as being reassuring about the existence of the ophthalmic surgeon in the future, patients are still going to choose to have an experienced, fully trained, ophthalmic surgeon perform their surgery.
Most people wouldn’t choose their family physician to do their cataract surgery, or their heart transplant or their total hip even though they’re legally allowed to do it.
Many institutions probably wouldn’t even give them privileges, so I think it’s more than just legislation. I think in the end it’ll be patients choosing the surgeons.
But maybe you don’t want to be the one who has to spend a half an hour doing the refraction and programming the adjustment laser and correcting the -.75D, +.50D to plano. You might want to delegate that.
We might get much more efficient, but the young surgeon is going to have to manage twice as many cataracts. New things keep happening. For example, I can imagine continued advances in glaucoma making glaucoma more of a surgical disease.
We can imagine advances in refractive surgery and therapeutics and refractive collagen cross-linking. If we add all the procedures up, the “ophthalmic surgeon” is going to be very busy, in my opinion. Which is a good thing.
KD: So should we be training more ophthalmology residents to plan for this increasing demand? Should we open more residency programs or increase the numbers of trained surgeons?
RL: Well, there are a couple of issues. No. 1 is that nobody wants to pay for education. So, when you go and try to get a new resident funded in any subspecialty, it’s hard to get the funding. I think what will happen is the same thing that has been happening over the last 45 years.
We’re going to learn how to be more efficient and hire appropriate support, such as PAs. We have three of them in our group and 12 optometrists as well.
One of the PAs actually practices much like a medical ophthalmologist with meaningful training and then the other two are more involved in histories and physicals for surgical patients.
KD: What do you think about the future of the femtosecond laser? The debate is ongoing regarding comparisons between femto vs. traditional cataract surgery. Do you think we’ll still be using a femtosecond laser in 10 years?
RL: I think it’ll be different than it is today. I think as an elective refractive tool used for a premium upcharge, there will be a role for femtosecond. I think it will fit in that category of premium upcharge and for refractive purposes.
We’ll just have to see what other refractive tools come along that might achieve the same goal for a lower cost. I think that will put pressure on femtosecond lasers.
It’s still uncertain where we’ll be with femtosecond lasers in a decade, but they are continuing to gain in usage. Surgeons are finding it useful today in that premium channel group of patients.
KD: So you don’t think the femtosecond laser will ever be considered the standard of care and be covered by insurance companies?
RL: No, because I think that’s going to go away, this whole idea of getting paid a facility fee per procedure, which is what we’re so used to that we can’t imagine it would go away.
You could be trying to fight to say we want to include femtosecond lasers in our standard surgeries so we want an increased facility fee. I really think what third-party payers are going say is, “We don’t care what you use, but this is the amount of money we’re going to give you to do this many cataracts.
If you find that it makes you able to do cases faster or to reduce your complication rates, then use it because you’re going to have manage your own complications as well.
So, if the patient returns to the OR for a second procedure or if there are other issues, you just won’t get paid extra for that.
You’ll just have to take care of those patients.” That’s why, for example, Kaiser still uses nonsteroidal anti-inflammatory drops.
They did a study that showed it reduced the complication rate, which was not only the right thing to do but also economically viable.
As surgeons, we’ll be making that decision. We will be the stewards of the bucket of money that we’re given, and we will have to pay all our employees and pay to buy all the equipment (such as a femtosecond laser).
If we want to have an income, we’re going to have to manage the bucket of money, so there is something left over. If we’re bad stewards, we’ll be at risk.
KD: Everyone is talking about using less drops or no drops for cataract surgery. What should be done to replace drops?
There are also some compounding issues related to the use of intracameral injections. Are you still using drops with your cataract surgery? What do you see for the future of drops in cataract surgery?
RL: I am doing what my good friend, Vance Thompson, calls “drop a day.” I eliminated topical antibiotics from my practice several years ago; I now use intracameral compounded moxifloxacin. I believe I’ve chosen wisely who I work with for compounding.
I believe the data is very convincing that there is a fivefold reduction in risk with intracameral antibiotics. ASCRS (its research council) is working together with the National Alliance and the VA and others are trying to do the appropriate study to get an FDA approved product here in the United States.
I’m also a believer that steroids and NSAIDs are synergistic, and I’ve been using an injectable steroid at time of surgery as well. Now we’ll have two FDA-approved products for post-surgical inflammation: Dextenza as a punctal plug (dexamethasone ophthalmic insert; Ocular Therapeutix) and Dexycu (dexamethasone intraocular suspension; Icon Bioscience Inc) as a microsphere injection.
I believe both will get pass-through status, which will make it free to the surgeon and free to the patient. I’m going to investigate those options because I’m paying for the steroid injection and for the antibiotic injection.
So, I’ve eliminated topical steroids and antibiotics, and I only prescribe an NSAID, using a once-a-day branded NSAID when my patients can afford those.
KD: Which injectable steroid are you using? And how are you injecting it?
RL: For a period of time, I injected intravitreal steroids, but now I just inject dexamethasone into the anterior chamber. I actually have a compounded formulation composed of moxifloxacin, dexamethasone and Ketorolac that I inject at the end of the case.
It’s amazing how good the eyes look on the first day. Of course, those drugs are all gone in 24 hours. I have found with that, all I need is a topical NSAID afterwards.
Routinely, you can have postoperative breakthrough inflammation, so you can always add a topical steroid later, but I can’t remember having done that in the last year. However, I am going to look at Dextenza and Dexycu because I would like the steroids on board longer than just 24 hours.
KD: Does the compounded formulation that you’re using blur the vision or ever cause a pressure spike?
RL: No, because it’s gone in 24 hours. You have a very minimally inflamed eye in the first 24 hours, and the eye looks great on the first day because you’ve got lots of steroid and NSAID onboard along with your antibiotic prophylaxis.
I haven’t seen a problem, but you do have to make sure that you are using a compounded formulation that has the right concentrations. I was using an intravitreal injection for a period of time, but while it works well I didn’t like the floaters and the blurry vision.
I was doing transzonular injections, and while I didn’t personally have complications I heard of others with complications. If I did enough of them, I probably would’ve had complications too. In those cases, I did have IOP spikes.
When you have an injectable, long-acting steroid, such as triamcinolone, onboard for four to six weeks, some of those patients have pressure spikes. But pressure spikes have gone away because I’m just injecting dexamethasone at the time of the surgery and it’s gone in 24 hours.
KD: There have been a lot of serious compounding issues in the news through the years. Do you ever worry that perhaps if there were a compounding issue, that someone could testify that there was a safer, well-established alternative?
RL: I think that’s a legitimate issue to be concerned about. That’s why I think it’s necessary to choose your compounding pharmacy carefully. I’ve gotten comfortable with the manufacturer I work with, so the risk-benefit ratio is reasonable in my practice.
I think the oversight is higher at a 503B compounding pharmacy than it is in a generic pharmacy, and many of us are certainly using a lot of generic drugs.
KD: You also mentioned the possibility of cataract surgeries someday being performed in an office setting — maybe even in the mall or during a person’s lunch hour. As practice patterns change with the increased load on surgeons, do you see cataract surgery being performed in that way?
RL: I think the office surgery trend is all about cost, and the regulatory burdens placed on hospitals or ambulatory surgery centers are meaningful. I don’t think the operating suite is any different in quality.
I believe Kaiser operates in an office-based surgery center and that the quality of air exchange, cleanliness, everything is at the same level as it would be in a typical ASC or hospital OR. However, the regulatory oversight is lessened, which reduces costs.
As we are given that bucket of patients and a bucket of money, we’re going to be looking for ways to reduce costs (of course, while maintaining patient safety).
It would be the unusual surgeon who was given a bucket of patients to take care of and a bucket of money that would choose to go to a hospital and pay $1,600 per case for the right to be able to do a cataract surgery vs. doing it in an ASC at $900 vs. perhaps doing it in an office for maybe $300 or $400. So, it is going to be an economic issue.
However, I would imagine that if you were the surgeon and you were blindfolded, when you suddenly had the blindfold taken off in the operating room, you wouldn’t be able to tell whether you were in an actual ASC, hospital or office, right?
The equipment would be equally good, the ancillary personnel would be equally good, the cleanliness would be equivalent, the air exchange would be equally good and you wouldn’t know where you were. It’s just going to have a different name on the door.
KD: Very good point. As we look at the future of cataract surgery, we also need to take a look back 30 to 40 years ago for a moment to recall the hospital admissions for a week when cataract surgery involved lengthy incapacitation with sandbags to maintain stable head positioning.
So, if we could make that much progress over the past 30 to 40 years, it’s interesting to think what cataract surgery might be like in 30 or 40 years with this rate of progress.
RL: We’re going to get more and more efficient. Additionally, our friends on the pharmaceutical side are going to work hard to retard or reverse the development of cataracts.
While I don’t think this will impact any surgeons finishing their training today, I think the day will come when we may well have medical therapies that can reduce the number of patients who develop visually significant cataracts.
On the other side of the story, I think more and more patients will opt for lens-based refractive surgery as the best way to treat their refractive errors. We may find ourselves doing most surgery before the patient actually develops a cataract, and it may then be primarily cash pay.
It won’t matter if patients ever develop cataracts. And perhaps we’ll even learn how to retard the development of presbyopia, as well.
There are things that may be totally disruptive that we would have difficulty predicting. But, as far ahead as I can see, and I would say that’s about 30 years, I think there are going to be more cataracts to do every year, both in the U.S. and globally. But, the day will come when the curve could go back the other way.
KD: I think you were referring to the Science article about the lanosterol product in dogs last year. It stabilized cross-linking of the alpha-crystallins in the lens.
I always wondered what the side effects might be to the surrounding structures (like the zonules). Do you think we’ll have those drops within the next 10 years?
RL: I would say that if we understand the process of pathogenesis, there probably will be attempts to pharmaceutically modify the process of cataract formation over time. But there are so many cataracts in the incubator right now that it’s not going to matter to most of us.
However, the day will come when we probably will either retard or reverse cataracts and presbyopia. To me, that’s farther away. Thirty years or so.
KD: Is there anything else that you think is in our future as cataract surgeons?
RL: In the next decade, surgeons will probably find themselves doing a lot of bilateral, same-day, sequential cataract surgery. U.S. surgeons will find themselves doing primarily phacoaspiration, and there may not even be an emulsification amplifier on the machine they’re using — that could simply have a disposable handpiece.
They will have an adjustable, accommodating, interactive lens for the patients who can pay extra money. The biggest unmet need that I want to see solved (and I don’t know if we’ll make it in a decade) is the elimination of posterior capsular opacity. I think not enough is being invested in that area.