Good Nutrition & Cataracts
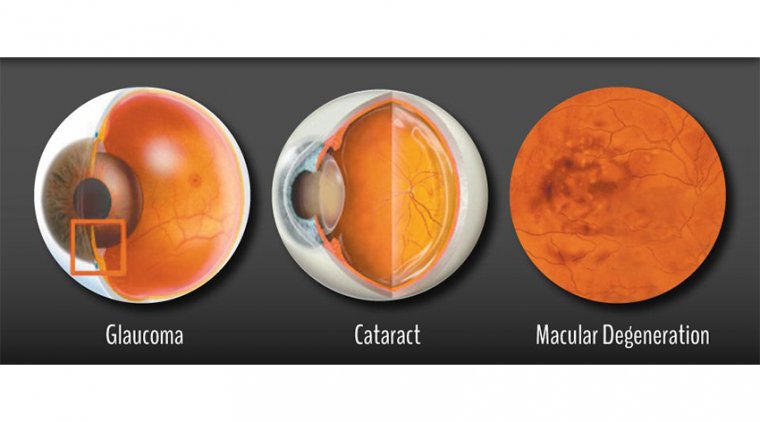
Cataract is defined as any visible opacity within the otherwise clear crystalline lens of the eye. Cataract can be further classified as cortical, nuclear, or posterior sub-capsular, depending on the anatomical location of the opacity.
Globally, over 80 million people are visually impaired due to cataract, however cataract-associated blindness shows significant geographical variation, accounting for less than 22% of blindness in high-income countries compared to more than 44% in South East Asia.
Age is the most significant risk factor for cataractogenesis. As the lens ages, conformational changes to lens proteins occur with subsequent aggregation, leading to a progressive loss of transparency and associated vision loss.
Oxidation reactions within the lens are thought to be a key factor in this process and there has been a significant amount of research on the role of antioxidant nutrients for preventing or slowing the progression of cataract.
Observational data suggest that the risk of cataracts can be reduced by a diet that contains optimal levels of vitamins C and E, the carotenoids lutein and zeaxanthin, and the daily use of multivitamin supplements.
However, RCTs that have compared antioxidant vitamin supplements (beta-carotene, vitamins C and E) to an inactive placebo or no supplement have been unable to detect any effect on the incidence or progression of cataract.
The tear film is the most important refracting surface of the eye, and improving it can increase a patient's quality of vision.
Cataract surgery deleteriously affects the ocular surface due to the neurotrophic effect of the corneal incision and the use of topical medications containing preservatives that can contribute to the development of dry eye disease.
More than 50% of patients who undergo cataract surgery may experience dry eye postoperatively.
Limbal relaxing incisions and excimer laser photoablation for overcorrection during refractive cataract surgery exacerbate the denervation and substantially increase the risk of ocular surface disease.
Improving cataract surgery patients' tear film is even more important when one considers that some refractive IOLs reduce contrast sensitivity.
Ocular surface disorder (OSD) is present in the majority of cataract patients; sometimes the signs are distinguishable prior to surgery and sometimes the symptoms appear following surgery.
Undetected and untreated, signs and symptoms can cause significant variability in preoperative measurements as well as inhibit rapid healing following surgery.
Thoroughly screening and potentially treating patients for OSD can mean the difference between a happy or unhappy patient. Untreated OSD will result in suboptimal outcomes and decreased patient satisfaction.
Ocular Surface Assessment
Every patient undergoes a comprehensive evaluation as part of the cataract consultation. Doctors use a variety of subjective and objective diagnostic tests to identify OSD or other structural deformities.
All patients receive corneal fluorescein and lissamine green staining, and they also are tested for inflammation levels.
Where the tear film is unstable, we watch for conjunctivochalasis or entropion and ectropion. Dropout areas, irregular topography, measurement inconsistencies, and abnormalities in tear film tests all can signal OSD, and, in our opinion, are reason to pause and treat the patient before proceeding with surgery.
Typically, we will see a patient back in 3 weeks and repeat testing. Using comparative topographies, we confirm corneal stabilization so that the patient and I are comfortable with the measurements.
We also look at the surface asymmetry index, which tells how asymmetric the corneal astigmatism is, and at the surface regularity index. These provide the topographic standpoint of the cornea and guide us if we should move forward.
We also look at how the numbers change in response to treatment. For example, we will look at the change in Ks. Once we see 0.25 D or less between measurements, we are satisfied that the ocular surface is stable and we can proceed to surgery.
Treatment For All
As part of our approach to optimizing the ocular surface before cataract surgery and to improve comfort postop, we require all premium lens patients to start taking a nutritional supplement containing the anti-inflammatory omega fatty acid GLA and other nutrients after their first measurement.
We also recommend HydroEye (ScienceBased Health) because it demonstrated in a clinical trial increased corneal smoothness, decreased inflammation, and improvement in the symptoms of OSD. All of these options are important for cataract patients.
For patients requiring treatment beyond nutritional supplementation, topical immunomodulators, such as lifitegrast or cyclosporine, are usually well tolerated and produce long-term improvements in the ocular surface.
In eyes with significant levels of inflammation, patients may benefit from a brief treatment with a corticosteroid. In addition, punctal occlusion may be utilized to address aqueous tear deficiency.
Patients with crusting blepharitis undergo mechanical debridement, short-term antibiotics, hypochlorous acid treatments, or a combination of these to remove inflammation-causing bacteria on the eyelid.
Once patients have been taking nutritional supplementation for 2 weeks and any other necessary OSD treatment has been performed, they return for a second set of keratometry readings and to proceed with cataract surgery.
We have our patients continue nutritional supplementation and an immunomodulator, if they were using one, until cataract surgery has been completed in both eyes.
Two weeks following the second surgery, we give patients the option to taper down the supplement and see if their eyes continue to be without symptoms.
Many of our patients with OSD notice a negative change if they discontinue the supplement and choose to continue because of the benefits they see, including better visual quality and an improved level of comfort.
Be willing to wait
When patients understand that we need a healthy ocular surface in its natural shape to get the best surgical outcome, they rarely push back. Symptomatic patients are especially understanding.
They are experiencing irritation and visual fluctuations and recognize that this is a consequence of degradation, not cataract. Overall, patients want the best results.
The “wow” factor
Patients with premium lenses have high expectations, and failure to deliver can stir up frustration. Managing the ocular surface on the front end is key to producing a “wow” factor postoperatively.
First, eliminating residual refractive error is essential when using any multifocal IOL. We always measure the cornea 4 ways, and, ideally, the numbers will coincide.
In patients with OSD, this will not be the case. We frequently get different measurements on the same eye. Moreover, this is an objective test, and it is a red flag to us that we need to improve the cornea surface to obtain the most precise measurements.
If not, we are probably increasing the likelihood that the patient will come out of surgery with residual refractive error.
Even without residual refractive error, ocular surface discomfort and visual fluctuations can create general health anxiety that may shape the patient’s perceptions about the procedure.
By taking precautions to ensure the cornea is in optimal condition prior to surgery, we can create a more resilient ocular surface and reduce postoperative keratopathy and negative visual fluctuations.
A proactive approach delivers the best outcomes
Proactively optimizing the ocular surface through a combination of nutraceutical supplementation and topical drop therapies such as lifitegrast or cyclosporine gives us more confidence in the preoperative measurements, leading to better results and patient satisfaction with their premium procedures.
In conclusion, it is a very dramatic effect when a patient experiences quality vision on day 1, and by day 5 they are able to read off their phone in low light.