Combining Diagnostic Data to the OR in Cataract Surgery
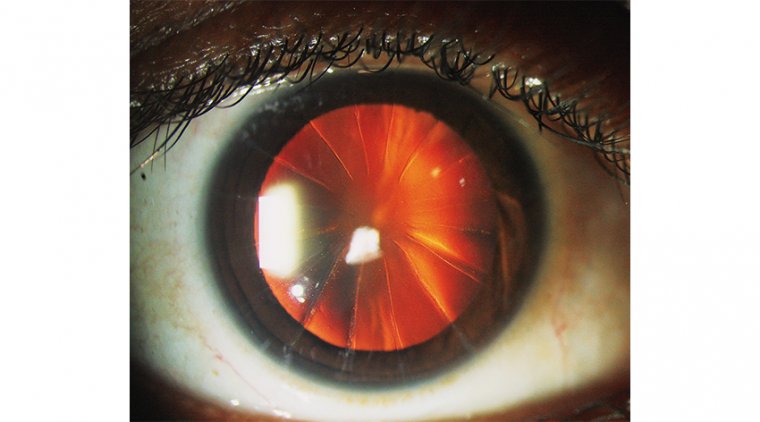
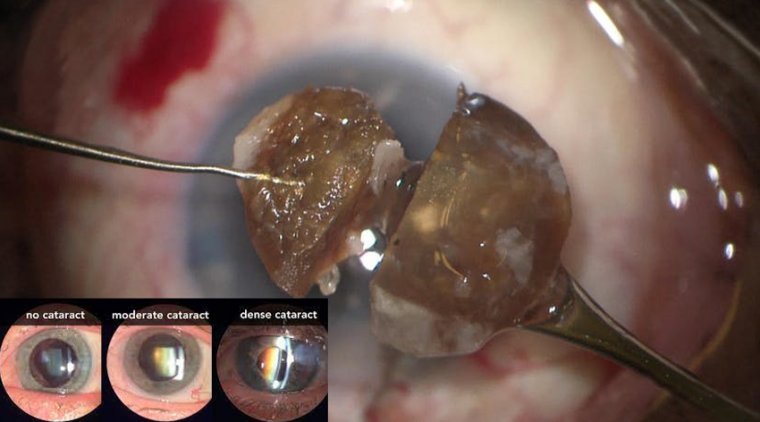
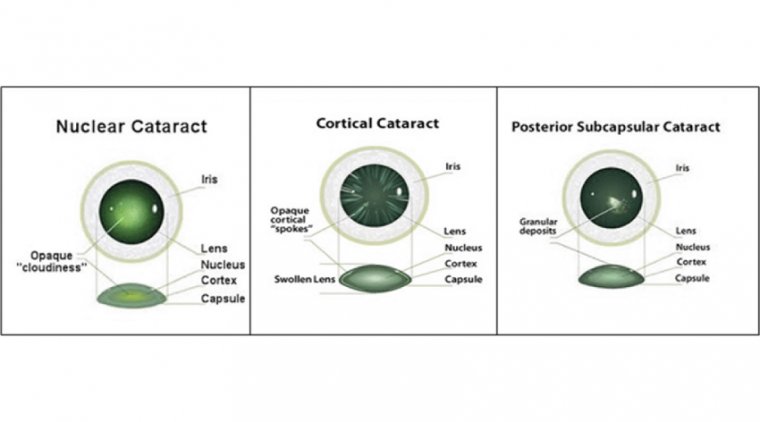
Cataracts develop when proteins accumulate in the lens, eventually resulting in cloudiness and decreased vision. This occurs naturally as one ages, and may be exacerbated through trauma, radiation, medications, and systemic diseases.
Symptoms experienced are fading of colors, glare, diplopia, sensitivity to bright light, and impaired night vision. Without treatment, cataracts continue to progress, eventually impacting quality of life. Fortunately, vision loss due to cataracts can be restored via corrective surgery.
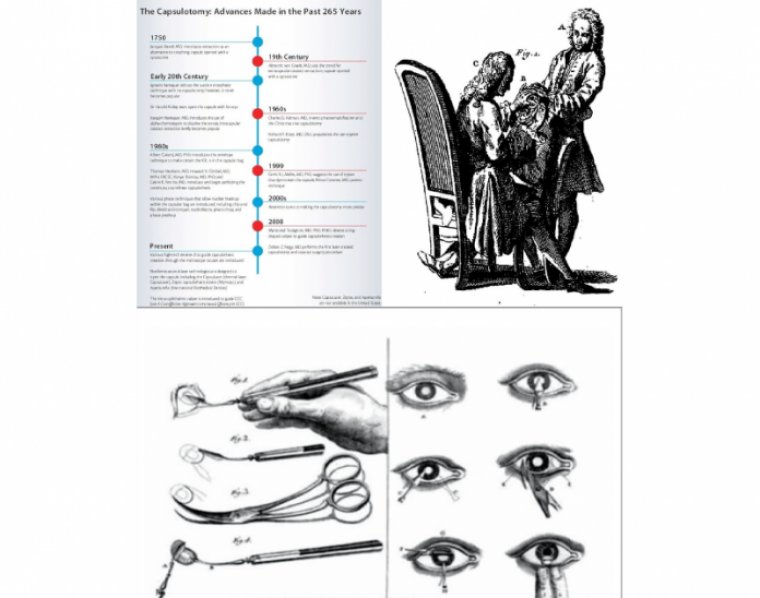
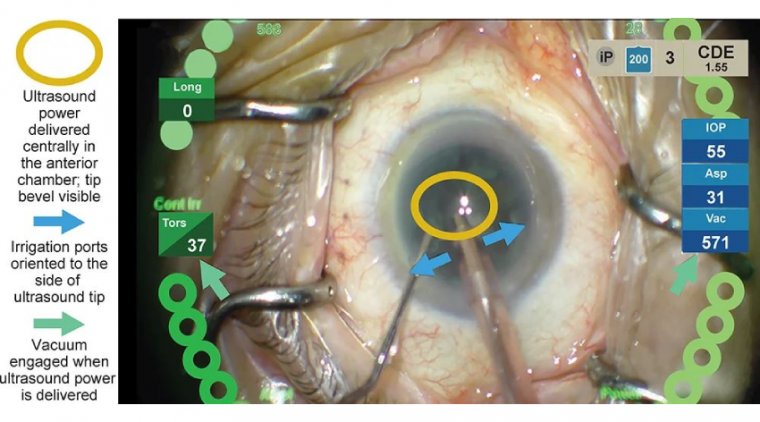
Cataract surgery requires extensive preoperative planning to select an intraocular lens (IOL) of proper power for the eye undergoing surgery.
To perform this calculation, a detailed ocular exam is required, and ocular biometry, including axial length, anterior chamber depth, lens thickness, corneal white-to-white measurements, and keratometry must be performed.
The required formulas for performing IOL calculations are often integrated into the same diagnostic instruments that perform measurements, which create a report, allowing surgeons to choose a lens power for each IOL model being considered to achieve the desired spherical equivalent refraction.
However, patients who have undergone prior refractive surgery and those who require toric IOL correction or incisional keratotomy may require additional calculations performed with special formulas, such as the Barrett True K or the Barrett Toric Formula, and these formulas do not uniformly reside on biometry machines, necessitating transfer of the data to a separate system for surgical planning.
This transfer of data introduces the possibility of transcription errors and consumes significant time. Considering that errors in transcribing numbers from one platform to another are possible, manual transcription of information critical to the refractive outcome is certainly not ideal.
A thorough preoperative workup also requires evaluation of tear film and ocular surface, endothelial cell count, optical coherence tomography (OCT) of the macula, and other diagnostic tests.
To review these documents during surgical planning generally requires accessing the diagnostic images in a paper chart or through a digital image management system that again is a separate system from that used for lens power calculation or toric calculation.
When it comes to learning new technology for cataract surgery, the time you spend understanding an unfamiliar system should have a handsome payoff for staff , surgeons, and patients. As a technician, you can gain such a payoff with systems that connect diagnostic data to the OR.
The benefits come in such forms as time saved, errors reduced or eliminated, and outcomes analysis enhanced. Here, we take a closer look at the advantages these systems provide.
First, let's learn how they work. Uploaded data Cloud-based systems upload data directly from diagnostic devices into the software, eliminating manual transcription of information.
For instance, at The Eye Associates, Sarasota and Bradenton, FL, a Zeiss Veracity system connects to an IOLMaster 700 (Zeiss) biometer, Cassini topographer and other devices, according to Cathleen McCabe, MD, medical director.
The Zeiss Veracity system is part of the Zeiss cataract workfl ow solution. Similarly, at Harvard Eye Associates in Laguna Hills and San Clemente, CA, an Alcon Smart Solutions system — the SMARTCataract application connects to an IOLMaster.
Once the data is in the Veracity system, Dr. McCabe and her technician can choose which formula she wishes to use for calculations; once complete, this forms a plan in the Surgery
• May/June 2022 tem for the cataract surgery. Then, she can view a map of the eye and other information, such as where she plans to orient a toric lens or where the limbal relaxing incisions for astigmatism correction would be; the IOL power and type; and backup lenses.
That summary can be used in the OR so all staff know the plan. "Preoperative testing data can be automatically uploaded into the Veracity planning software and used to make a customized plan for the patient that isn't going to have the added effort and possible errors of a person having to enter that data in for each of the patients for each piece of the testing equipment," notes Dr. McCabe.
Similarly, the Alcon system "allows you very quickly to go through information that is complex and do so without the worry about humans transferring information manually from one location to another, which is a source of potential error," says John Hovanesian, MD, owner.
One stop for calculations At The Eye Associates, Dr. McCabe utilizes her technician and lead biometrist, Serina Tindell, COA, to assist in planning her patients' surgery and analyzing their outcomes.
"Having data transferred from the IOLMaster 700 biometer to the Veracity system means there is much less room for error," says Ms. Tindell.
What's more, Ms. Tindell says that you can do all the IOL calculations on the Zeiss system. For instance, for a toric patient who was post-LASIK and wants to correct an astigmatism, Ms. Tindell previously would have to consult different calculators in different places.
In contrast, the Veracity system will run various formulas automatically, such as the Barrett toric or the Barrett Universal II calculations. "You have the ability to run several different formulas all in one place," Ms. Tindell says.
"It's like a one-stop shop as far as the calculation process is concerned." Time savings are notable.
For the post-LASIK patient who wants astigmatism correction, Ms. Tindell estimates it would take 15 minutes to enter the patient data, run the formulas, and review them with the surgeon without the Zeiss Veracity software.
With Zeiss Veracity, that time is reduced to about 5 minutes, she estimates. The practice uses the Zeiss system for all cataract patients.
Likewise, at Harvard Eye Associates, before the Alcon system, Julie Trotman, patient care coordinator, would have to manually input data from the IOLMaster into various calculators to determine the correct diopter.
With SMARTCataract, she will indicate in the system the lens required and the surgeon can then review the information and choose the correct diopter. That makes the process simpler for her as well as the surgeon.
"They don't have to put a lot of thought into it and look at all of these other programs to decipher which lens they're going to put in the patient's eye, because the computer system does it for them," Ms. Trotman says.
With the Alcon system, she estimates that she saves 10 to 15 minutes per patient. Before the Alcon system, theirs was strictly a paper practice for cataract calculations, says Jackie Schroeder, lead technician, NVISION Miramar, Ventura County, CA. Ms. Schroeder is based out of the Camarillo location.
"Since being able to use this new system, it's cut down the time that I spend trying to get surgeries planned," she says. "By having all my information right in front of me, I'm not flipping papers back and forth.
It's been super helpful." From 20 minutes per plan, Ms. Schroeder now spends about 7 minutes per plan, she estimates. Communication with OR With the Alcon system, the surgeon can much more easily make changes on the fly in the OR, says Ms. Trotman.
Prior to Alcon, the surgeon would have to call the clinic from the OR and have Ms. Trotman redo calculations with the IOLMaster for a different lens.
"If the doctor isn't able to put in a premium lens for some reason, for instance the zonules are loose or longer haptics are needed, he's able to change the lens and choose the power right then and there, instead of having to call us over at the clinic," she says.
The surgeon can simply consult the SMARTCataract application right in the OR. Easing outcomes analysis After surgery, these systems can help with outcomes analysis to gauge the results of procedures.
Without a system like Veracity, notes Ms. Tindell, outcomes analysis can be a tedious, time-consuming process of following patients and reviewing their refractions. Part of the work involves eliminating patients with pathologies such as retinal or corneal disorders.
The Veracity system, says Ms. Tindell, allows exclusion of those patients with pathology and makes it much easier to review patient data.
"It literally plots data points on a graph showing you how close your surgeon was to their target refractions," Ms. Tindell says.
"You can review patients who had a specific lens model implanted, and, in doing so, you can personalize the A-constant for each of the lenses after having a large enough data group.
Personalizing your surgeons' lens - A-constant will allow significant improvement and accuracy in your patient outcomes.
So far, in using the postoperative data analytics with Veracity, it takes significantly less time than it did previously." Similarly, at NVISION Miramar, Ms. Schroeder expects the Alcon system to save her up to 8 hours every month by streamlining outcomes analysis.
Every month, she finds patient 1-month post-op data in the EHR system, which she then manually enters into the Alcon Optiwave Refractive Analysis (ORA) system. The ORA system optimizes the A-constants so the surgeon can improve outcomes.
Worth the effort "I'm working with numbers all day long," says Ms. Schroeder. "I'm keying things in and it's very easy, as we're human, to have a typo here and there. Having it all just in a system where it's there and cutting that risk of errors is a huge deal."
Ms. Schroeder says it took about a month to feel comfortable with the system. But once you get through the training and trust the system, she says, the system will save time and reduce errors. "It's definitely going to be worth it."