Dealing with Complex Pathology in Cataract Surgery
Although cataract surgery almost always goes smoothly, the fact that it’s performed on millions of individuals every year guarantees that any cataract surgeon will encounter plenty of challenging cases over time.
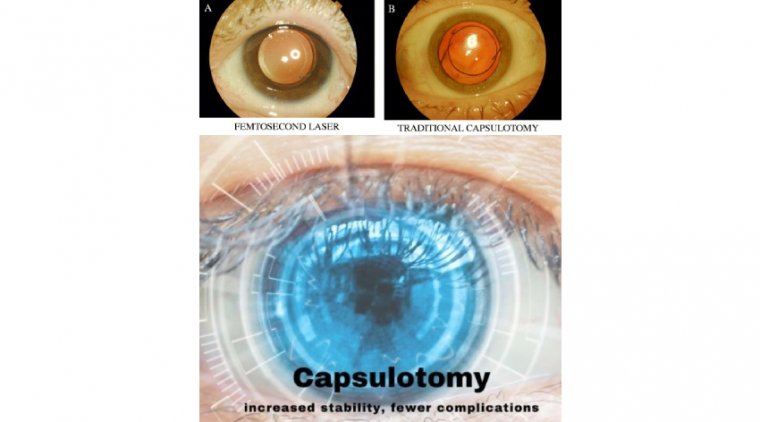
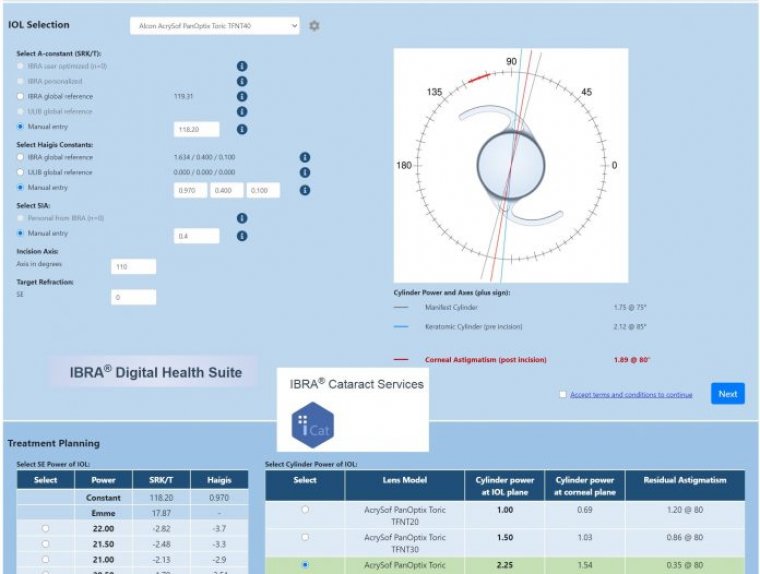
Modern cataract surgery provides a high level of efficacy and safety, incorporating numerous technological innovations, such as femtosecond laser technology or 3D visualization, as well as advances in intraocular lens (IOL) technology with the development of special or premium IOLs, such as aniridia IOLs, toric IOLs, or multifocal IOLs.
As a result, unparalleled visual outcomes can be achieved for patients by using customized solutions for each individual patient.
However, there are an increasing number of anterior segment pathologies, which could complicate cataract surgery and compromise the expected visual outcomes.
Cataract surgery in the presence of these complex conditions requires a special approach, including modification of surgical techniques and/or the use of special IOLs.
Modern cataract surgery is generally a successful procedure. Recent advancements—which involve the use of pre- and intraoperative pharmacological protocols combined with optimal instrumentation—allow for well-tolerated and eff ective procedures in the vast majority of patients.
However, there are certain preoperative factors that increase the likelihood of complications in cataract surgery. These need to be managed eff ectively if we want the capsule to remain intact at the completion of surgery.
The small pupil presents one such challenging case for the ophthalmologist. When it is combined with the pathology of the zonular apparatus, the risks during and after cataract surgery increase even further.
Several techniques have been described in the literature for the management of insufficient mydriasis combined with zonular pathology, ranging from pharmacological to surgical strategies involving mechanical pupil dilation.
To avoid complications in patients, it is essential to enlarge the pupil while also stabilising the capsule to maintain its integrity.
Another option - When dealing with patients who present with inadequate mydriasis as well as compromised zonules, in recent years we have come to rely on the Malyugin Ring (MicroSurgical Technology; MST) together with the MST capsule retractors, Chang modifi cation.
We find the capsule retractors to be very useful in overcoming zonular weakness and giving support to the equator of the capsular bag. However, in some cases it is possible to use the ring to simultaneously address the small pupil and stabilise the capsular bag, giving us yet another option in treating these cases.
Let’s demonstrate our clinical reasoning and surgical technique with the help of a case study, as follows.
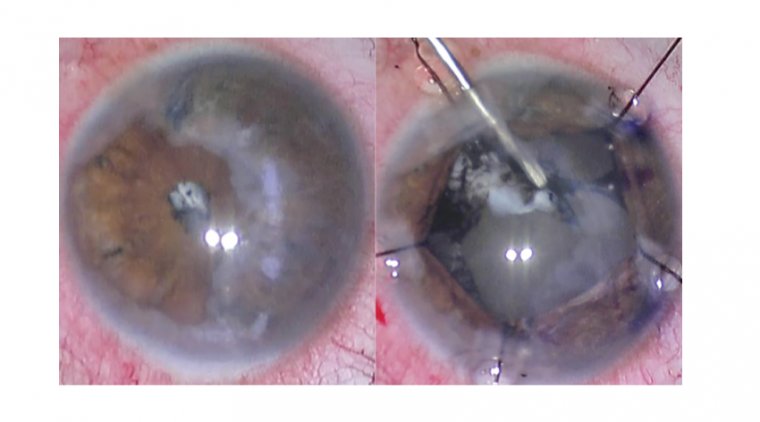
Complicated cataract A 75-year-old patient had a cataract complicated by pseudoexfoliation syndrome with sub-optimally dilated pupil. The patient has been taking the drug tamsulosin for several years to treat benign prostate hyperplasia.
Because the patient’s zonules were loose and the lens was mobile during the capsulorhexis procedure, my strategy was to use the ring to address the small pupil and to stabilise the capsular bag.
To perform the continuous curvilinear capsulorhexis, we used the 23G Seibel capsulorhexis forceps (MST), which feature a sharp tip and a rhexis ruler to allow for visibility and control during the procedure.
In many cases associated with a weak zonular apparatus, the lack of counter-traction on the capsule could unintentionally result in a smaller rhexis diameter.
A smaller rhexis may not only increase the risk of damage to the capsular edge during the procedure but may also cause capsular phimosis in the postoperative period.
Our approach was to use the ring to both stabilise the capsular bag and dilate the pupil, so I enlarged the rhexis to prevent the damage to the capsule that may occur while engaging the scrolls with the capsular edge.
The lens nucleus was fixed with the chopper to avoid excessive movement during the enlargement of the capsulorhexis. A 7.0 mm ring was inserted into the anterior chamber. We engaged the iris to support and enlarge it while simultaneously catching the edge of the anterior capsule with the scrolls of the device.
This was done bi-manually with the ring manipulator in one hand and the micro-hook retracting the capsular edge in the other hand. In these cases, you only need up to three scrolls for the fixation: if you try to use four scrolls, there might be too much stress placed on the capsule.
Because I was using the ring alone, I did not have the same stability at the capsular bag equator as with capsular hooks. Therefore, the area with the loose zonules needed to be carefully monitored.
One option is to continuously inflate the capsular bag with dispersive ophthalmic viscosurgical devices to create a viscoelastic cushion and prevent the aspiration of the capsule equator.
We then inserted the conventional capsular tension ring and was able to safely remove the last fragments of the lens by stabilising the capsular bag equator.
After removing the cortical material, I disengaged the scrolls of the ring from the rhexis and repositioned them to the iris to maintain pupil dilation. When the anterior capsule was released, we could implant a single-piece IOL in the capsular bag.
Finally, the ring was removed from the eye and triamcinolone acetonide suspension was injected into the anterior chamber to check for the possible presence of the vitreous strands.
Cases of complex small pupil cataract complicated by zonulopathy are particularly challenging. Surgeons need to carefully evaluate multiple factors, such as pupil size, rigidity of the iris, sphincter fibrosis and level of zonular weakness, among other considerations, to choose their strategy.
The Malyugin Ring 2.0 alone or in combination with capsule retractors helps alleviate complexities in these cases.