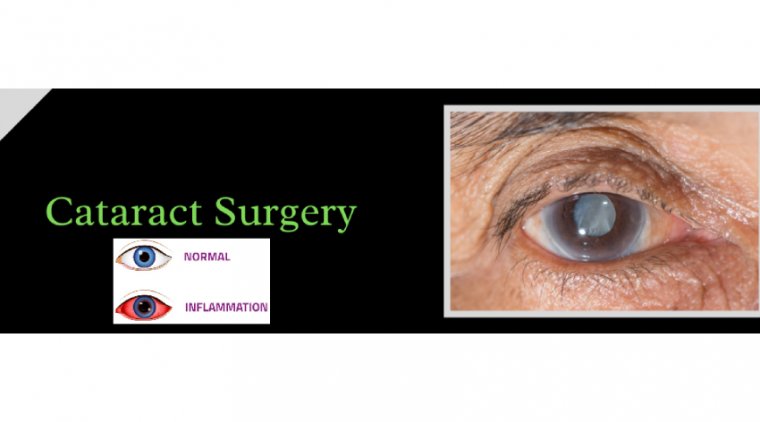
How to Minimize Inflammation After Cataract Surgery
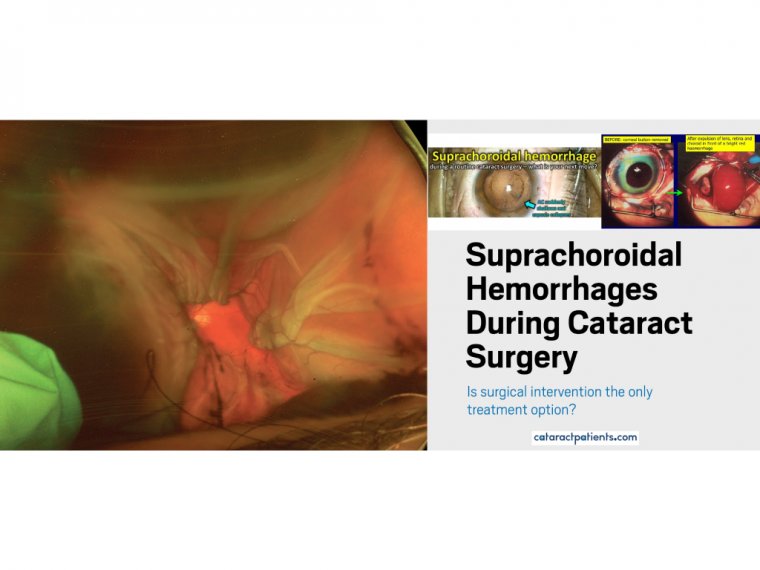
One of the keys to a successful operation is the prevention of complications, which, although rare and ranging from mild and transient to vision-threatening, still occur in approximately 5% of patients.
Infection, in the form of endophthalmitis, and inflammation, which can lead to cystoid macular edema (CME), are the 2 major complications of cataract surgery, requiring preventive measures.
Most physicians use a prophylactic perioperative regimen consisting of topical fluoroquinolones, corticosteroids, and nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce the risk for infection and inflammation.
Some patients may complain of slight discomfort after cataract surgery. It may range from mild to moderate discomfort depending upon patient’s sensitivity and type of procedure used for cataract removal.
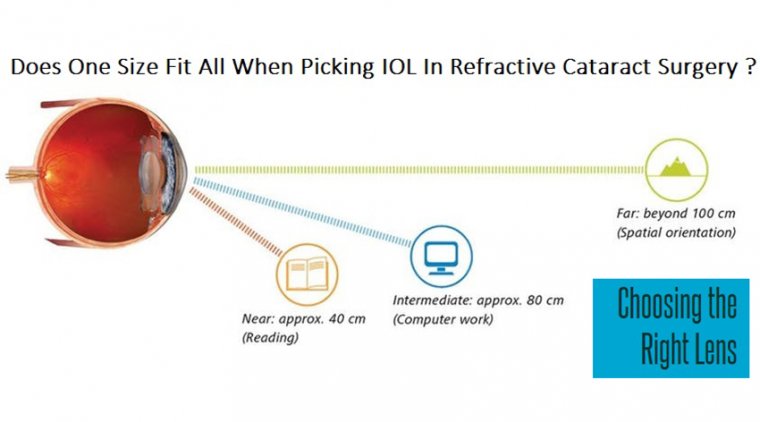
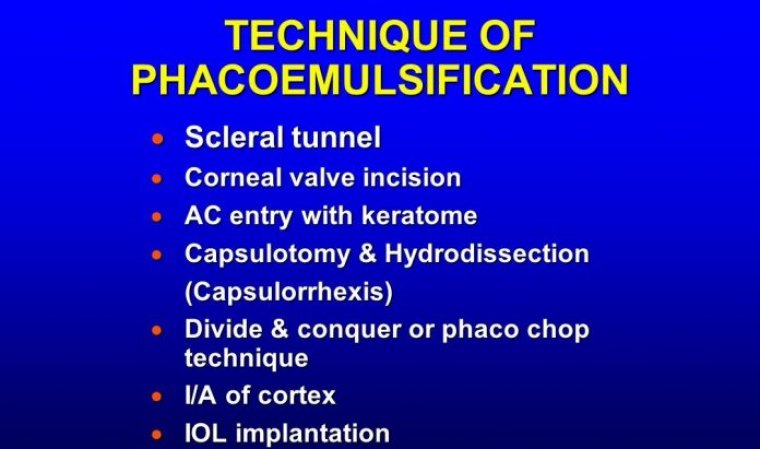
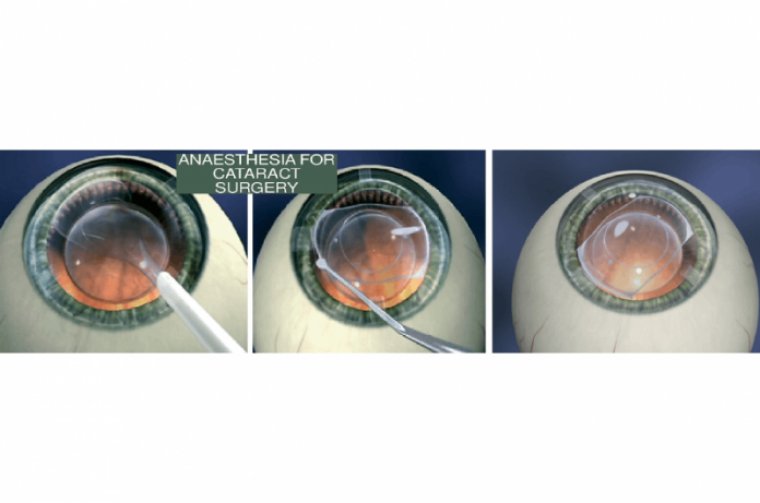
Cataract surgery has evolved into a minimally invasive refractive procedure. Incision over cornea (the front transparent part of the eye) is an important step in cataract surgery to get entry inside the eye and get access to the lens to be replaced.
This incision cuts multiple connections between neurons/nerves over that part of cornea. Patient might feel discomfort because of such incisions. Healing over this region per se can produce abnormal sensation.
Though superficial healing occurs within 5 to 7 days, ultimate healing response continues for 3 months on cellular level. This can also affect tear secretion. If patient is already suffering from dry eyes syndrome, surgery can cause extra discomfort to such patients.
There is minimal inflammation inside the eyes after cataract surgery/ any intra-ocular surgery, this inflammation itself can be a source of discomfort to the eyes.
With modern day cataract surgery, incidence of inflammation is very minimal but preexisting inflammatory condition like anterior uveitis, glaucoma, dry eyes can cause additional inflammation leading to more discomfort.
To prevent irritation after cataract surgery, certain medications are advised for particular time frame. These drops keep eyes moist and minimize redness/ inflammation. Lubricant drops after cataract surgery should be continued at least for 3-6 months and even after that if required.
Preexisting conditions like uveitis are treated first and then cataract surgery is advised to prevent post-operative inflammation.
Cataract surgery is done to improve the vision, mild discomfort should be expected after the surgery and such discomfort will get reduced within few weeks to months after the surgery. Those with pre-existing dry eyes should continue using the lubricating eye drops to minimize such occurrences.
Results of a prospective randomized trial comparing 5 medication regimens for controlling inflammation early after uncomplicated surgery show that beginning monotherapy with a topical nonsteroidal anti-inflammatory drug (NSAID) the day of surgery offered the best outcome for efficacy and safety.
The findings, presented by Jesper Høiberg Erichsen, MD, revealed that adding a topical steroid to the NSAID provided no benefit but could adversely affect intraocular pressure.
Initiating topical treatment 3 days preoperatively also conferred no advantage for better inflammation control, whereas a dropless approach using a sub-Tenon corticosteroid injection proved inferior to topical treatment.
Controlling postoperative inflammation is important for achieving a successful outcome after cataract surgery.
Surgeons generally prescribe an anti-inflammatory prophylactic regimen parallel to surgery, and recent meta-analyses have documented a beneficial effect of using a topical NSAID.
There are several questions about inflammation prophylaxis require investigation. Surgeons recommend that cataract surgeons consider using NSAID monotherapy as anti-inflammatory prophylaxis in uncomplicated cases.
Patients with a senile cataract were eligible for enrollment in the study if they were undergoing uncomplicated surgery and had no history of diabetes, uveitis, glaucoma, retinal vein occlusion, epiretinal membrane, retinal detachment, or advanced age-related macular degeneration.
A total of 470 patients were randomly selected in 5 equal groups to receive topical prednisolone and ketorolac started 3 days preoperatively, topical prednisolone and ketorolac started on the day of surgery, ketorolac started 3 days preoperatively, ketorolac started on the day of surgery, or a sub-Tenon depot of dexamethasone 2 mg/0.5 mL.
All topical drops were to be administered 3 times daily and continued for 21 days after surgery. After random selection, 14 patients were excluded, and 438 completed follow-up to the primary end point visit at postoperative day 3.
The mean age of the 456 patients included in the baseline data analysis was 72 years, and almost two-thirds of the participants were women. The primary outcome assessed change from baseline in anterior chamber flare measured on undilated pupils using a flare photometer (Kowa FM-600, Kowa Company).
For statistical analyses, the group that received the combination topical regimen started preoperatively was used as the control group. Median flare was 10.1 photon counts per millisecond at baseline in all groups, and it increased significantly at postop day 3 in all groups.
The greatest rise occurred in the dropless group, and the difference in change from baseline compared with the control group was statistically significant only in the dropless group.
“As another interesting result, it was found that only a few patients in the topical treatment groups [1.1%-3.4%] needed additional intervention to control inflammation, whereas more than one-third of patients in the dropless group needed rescue antiinflammatory treatment.
Minimizing the need for topical drops is desirable in older patients who may struggle with administration, but the dropless approach using the sub-Tenon injection did not seem effective for achieving that goal.
Anterior chamber cell count at postop day 3 was investigated as a secondary outcome measure. The mean value was 3.4 in the control group, ranged from 3.8 to 4.1 in the 3 other topical regimen groups, and was 5.5 in the dropless group.
Again, Erichsen noted that the only the difference between the dropless and control groups was statistically significant. Postop day 3 logMAR visual acuity measured with Early Treatment Diabetic Retinopathy Study charts was also evaluated as a secondary end point.
The results showed no significant differences between groups. Intraocular pressure, another secondary outcome measure, was found to decrease significantly after cataract surgery in all groups.
However, the drop was significantly less in the combination treatment groups that received a topical steroid compared with those receiving a topical NSAID alone and the dropless group.