Cataracts & Ocular Surface Disease Index (OSDI)
Cataracts & Ocular Surface Disease Index (OSDI)
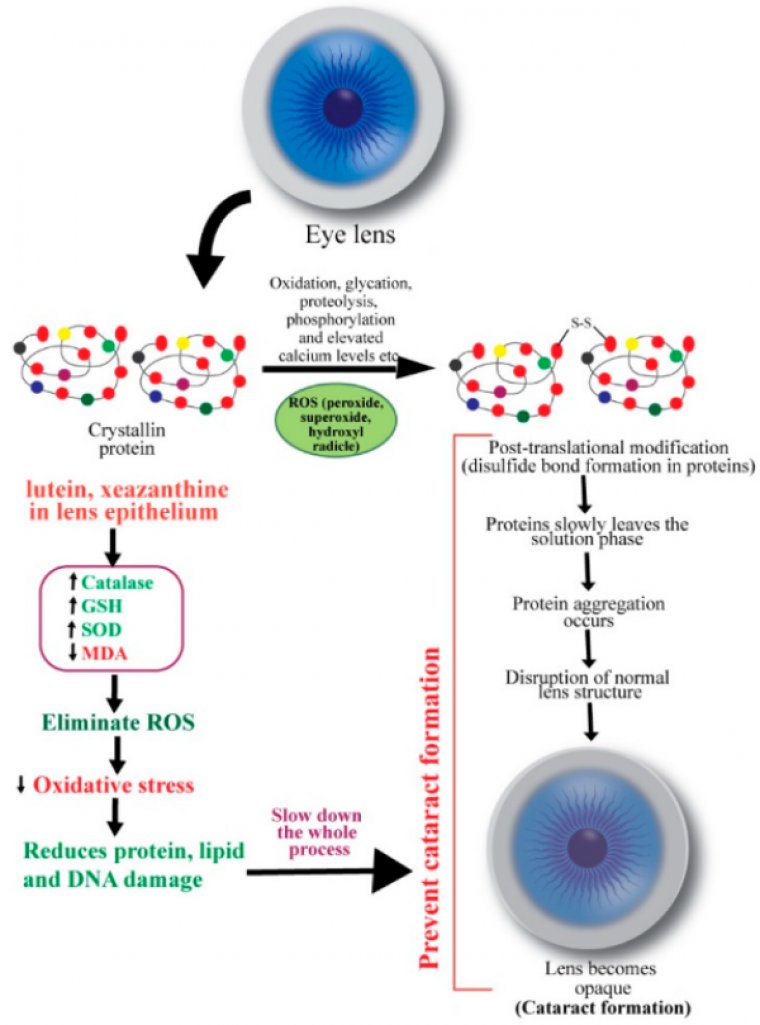
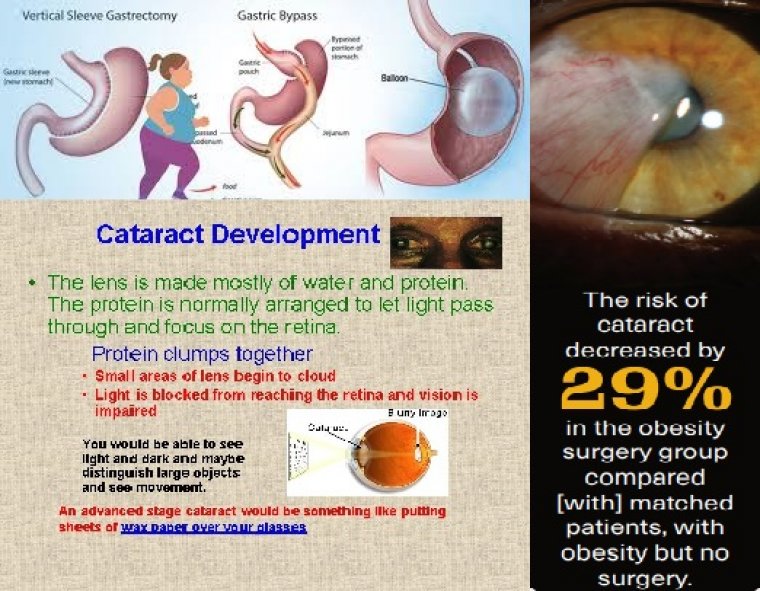
The ocular surface disease worsens most often after cataract surgery, multiple factors can contribute including transection of corneal nerves leading to loss of corneal sensations and impaired healing, damage to the corneal epithelium due to intense microscopic light exposure, prolonged irrigation of ocular surface with irrigating solutions, ocular surface irritation leading to an elevation in the inflammatory mediators and use of preservatives in topical anesthetic drops.
When dry eye disease (DED) is unidentified or inadequately treated prior to cataract surgery, it can adversely affect the surgical outcome for many reasons.
Preoperative lens measurements can be inaccurate in the setting of an irregular ocular surface, causing surgeons to implant the wrong type of lens, select the wrong IOL power, misalign a toric IOL, or even place astigmatism incisions at the wrong location.
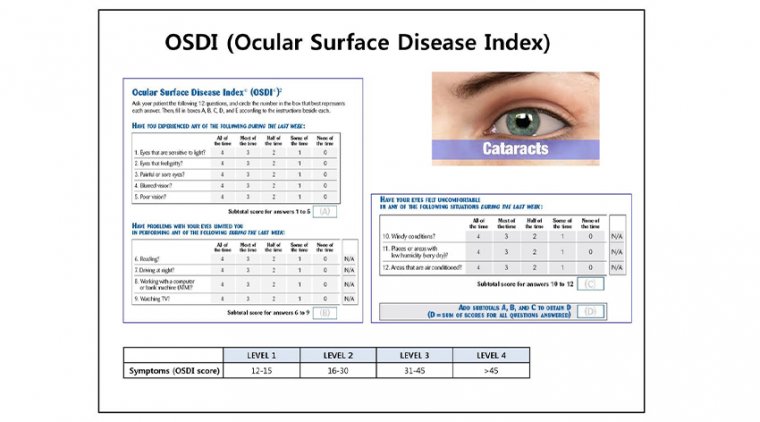
Moreover, because the signs and symptoms of dry eyes do not always correlate, a patient who preoperatively is asymptomatic but has a moderate to severe ocular surface disease index (OSDI) score can develop new visual symptoms in the postoperative period, which results in discomfort and overall dissatisfaction with the surgery.
Tutt reported that tear film irregularities reduce retinal image quality by 20% to 40%. Specifically, tear film irregularities induce higher order aberrations, diplopia, starbursts and shadowing; they all contribute to poor visual quality.
These points highlight the importance of identifying patient-reported dry eye symptoms prior to cataract surgery and optimizing the ocular surface. Furthermore, a greater proportion of patients report being “very satisfied” with their vision when there are no refractive errors.
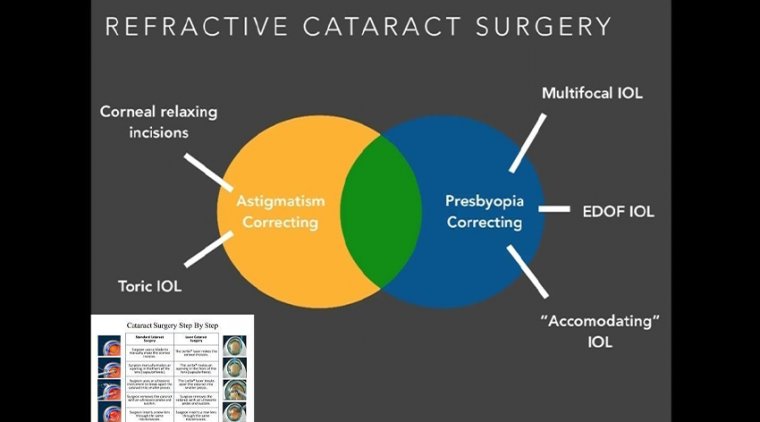
So, to reach 20/20 uncorrected at distance and near in presbyopic patients with astigmatism, many anterior segment surgeons are striving for increased precision at all touchpoints: preoperative biometry measurements, surgical finesse and refractive outcomes.
We are as well. Here’s how we identify and manage OSD prior to cataract surgery.
IDENTIFYING ASYMPTOMATIC PATIENTS
Abnormal-tear test results are highly prevalent among patients with minimal to no symptoms of OSD who present for cataract surgery.
The PHACO study (prospective health assessment of cataract patient ocular surface) showed that 87% of scheduled cataract surgery patients with clinical evidence of DED and had been diagnosed with it were asymptomatic.
Even mild OSD can lead to suboptimal refractive outcomes after cataract surgery, furthering the importance of preoperative diagnosis and treatment.
Not only do these studies point out the high proportion of DED in the cataract surgery population but they underscore the fact that clinical signs and patient reported symptoms do not always correlate, especially in the older cataract surgery patient population.
Therefore, clinicians might miss a diagnosis of OSD, especially if they rely heavily on unsolicited patient symptomatology alone.
The best way to identify these patients is to train staff to ask about symptoms. Various dry eye questionnaires can help, including SPEED, OSDI and SANDE.
Also, staff can ask a few simple questions:
- Does your vision fluctuate throughout the day or with certain focusing activities (reading, driving, watching TV)?
- Do you use artificial tears more than two to three times per day?
- Do you have any symptoms such as ocular fatigue, burning, foreign body sensation, irritation and so on?
Other topics to address during the preoperative exam include duration of screen time each day, occupational risk factors (computer work, reading, driving, exposure to sun or wind), chronic contact lens wear and hormonal replacement therapy.
If the patient responds “yes” to any of these questions, the next step is point-of-care testing.
DIAGNOSTIC TESTING
Point-of-care diagnostic tests produce an objective measure of tear quality. Tear osmolarity correlates with dry eye severity, and we can follow the value to monitor response to treatment.6
InflammaDry (Quidel) is our screening test of choice. InflammaDry evaluates the tear film for matrix metalloproteinase-9 (MMP-9) the inflammatory mediator elevated in dry eye conditions, which distressed epithelial cells release into the tears.
InflammaDry was found to be 85% sensitive and 94% specific in identifying MMP-9 in the tear. The presence of this inflammatory biomarker indicates the need to treat with anti-inflammatory agents such as cyclosporine, lifitegrast (Xiidra, Shire) or a short course of topical steroids.
It also provides a qualitative measurement to follow as we treat the dry eye. Additionally, the test device contains a helpful visual to show patients the pink line as a positive indicator for inflammation so that they can understand the pathophysiology of their disease and get on board with treatment.
Other point-of-care tests include TearScan (ATD) and TearLab (TearLab). Lactoferrin is a protein secreted into the tear film by the lacrimal gland’s acinar cells and plays a role in preventing ocular surface inflammation.
TearScan identifies low levels of lactoferrin (indicative of dry eye disease) with 83% sensitivity and 98% specificity. Tear osmolarity levels (measured with TearLab) over 308mOsm/L or a difference of more than 8mOsm/L between the two eyes correlates with dry eye severity.6
When one or more of these point-of-care tests are positive, we supplement lubrication of the ocular surface (which we do for all dry eye patients) with medications targeting the inflammatory component of the disease. We also follow these values over time to monitor the response to treatment.
SLIT LAMP EXAM
Point-of-care tests are valuable but do not replace a good slit lamp exam. An evaluation of the lid margin and assessment of the quality and rapidity of the meibum secretion are also essential for gathering information on the tear film’s lipid layer.
We express the meibomian glands with a cotton tip applicator to assess the quality of secretions (thick like toothpaste or thin like olive oil) and look for evidence of anterior blepharitis, including telangiectasias, eyelash scurf or Demodex.
Next, we assess the tear volume by measuring the tear meniscus height. Corneal and conjunctival staining with fluorescein and lissamine green can help identify damaged and devitalized surface cells indicating a lack of mucin in the tear film or corneal erosions and abrasions.
IMAGING
Useful tools for showing patients the physical signs of their pathology include meibography imaging of the meibomian gland architecture and slit lamp photos of cornea fluorescein staining.
Side-by-side photo comparisons of the patient’s photos to “normal” and severely “abnormal” can validate their symptoms and could even motivate some patients to adhere to a treatment plan, especially those who are asymptomatic but have moderate to severe signs of DED.
Allowing the patient’s accompanying family member to look through the slit lamp oculars (on low magnification) to see the “dry spots” also makes the disease more tangible and encourages increased compliance with treatment. Another useful visual includes measuring the tear meniscus height with anterior segment OCT.
If, at the cataract screening appointment, we find signs of abnormal tear film after our testing and exams, we initiate a treatment plan for the ocular surface. The patient returns for biometry testing.
After preoperative biometry and topography, we look at the mires on topography to further assess for irregularities in the tear film. If the placido ring mires are distorted or missing, then we treat the surface and repeat measurements prior to proceeding with cataract surgery.
When the cylinder axis or magnitude of astigmatism on the advanced biometer (IOLMaster, Zeiss) does not correlate with topography measurements, it raises our suspicion of inaccurate measurements.
DED TREATMENT
In patients with moderate to severe DED, we postpone surgery by weeks or months to allow time for the ocular surface to improve.
Or, when there is evidence of limbal stem cell deficiency such as whorled keratopathy, we will place a Prokera amniotic membrane, even when a frank epithelial defect is absent.
POST-TREATMENT AND CATARACT SURGERY
After DED treatment, we bring the patient back for repeat testing to get accurate data for IOL selection.
Similar to how we ask refractive surgery patients to stay out of their contact lenses prior to obtaining measurements, we treat dry eyes for three to four weeks before retesting to optimize the ocular surface.
We have seen significant cylinder meridian, magnitude of astigmatism and IOL calculation changes after aggressively treating dry eyes.
We provide counseling to every cataract patient and explain that dry eye symptoms can worsen or develop after cataract surgery, which is essential to set realistic expectations.
A variety of factors in the perioperative period contribute to exacerbating symptoms. Frequent administration of preserved preoperative and postoperative eyedrops damage the epithelial surface.
The corneal incisions made at the time of surgery disrupt the feedback mechanism that stimulates the lacrimal gland by the corneal nerves.
Prolonged exposure to the microscope’s light, aggressive irrigation of the tear film and frequent topical anesthetic on the day of surgery all traumatize the corneal epithelium and/or cause conjunctival mucous goblet cell loss.
DED identification and management are of utmost importance, especially as patient-driven demands for successful refractive outcomes are on the rise.
Cataract surgery alone exacerbates dry eye symptoms or “causes” new onset disease by unmasking overlooked, underlying dry eye. The cataract surgeon who proactively identifies and warns their patients of their disease is a hero.
In contrast, if dry eye goes unmentioned during the preoperative assessment and patients experience prolonged symptoms postoperatively, the patient will likely experience refractive surprises, disappointment in outcomes and overall dissatisfaction.