Diabetic Retinopathy & Cataract Surgery
Compared to non-diabetic patients, outcome after cataract surgery was reported to be worse in diabetic patients--especially in those with diabetic retinopathy.
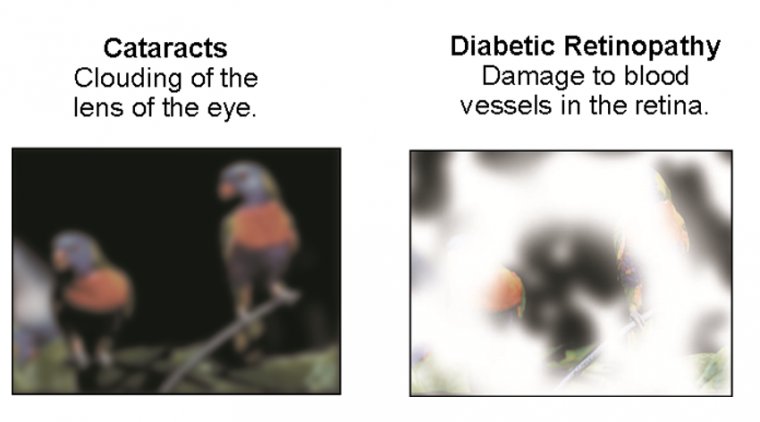
Cataracts and diabetic retinopathy (DR) are the leading causes of acquired blindness worldwide, which is further compounded by the fact that patients with diabetes have an increased risk of developing cataracts.
Thus, many patients with diabetes concomitantly have cataracts and DR. Although extraction is the standard treatment option for cataracts, it is also reported to worsen existing cases of DR, a microvascular complication of diabetes, leading to further vision loss.
It was postulated that cataract extraction may possibly lead to a breakdown of the blood-retinal barrier and the blood-aqueous barrier and enhanced intraocular inflammatory response, all of which may result in the occurrence of DR in patients with diabetes.
For this reason, current DR care guidelines also recommend measures of preoperative stabilization for patients with diabetes and existing vision-threatening DR who undergo cataract extraction.
These measures include optimizing glycemic control and performing panretinal photocoagulation preoperatively to better prevent postsurgery complications such as neovascularization and vitreous hemorrhage among this group of patients.
At some point, every ophthalmologist is going to have a diabetic patient walk into the office who is going to have a visually significant cataract. Diabetic retinopathy is the leading cause of vision loss among patients with diabetes and a primary cause of blindness among working-age adults.
As a result, the purpose of the study was to evaluate how diabetic retinopathy influences cataract surgery. The primary aims included studying preoperative risk factors, intraoperative complications, and postoperative outcomes.
METHODS
The study examined a retrospective clinical database study of 217,107 eyes that underwent cataract surgery at eight UK National Health Service hospitals between 2000-2015.
Of those eyes included in the database study, 138,100 were not diabetic; 41,059 were diabetic; and for the remaining 37,948, the diabetic status was not recorded.
Our methods for the evaluation of risk factors compared prevalence of preoperative risk factors and co-pathology between diabetic patients and non-diabetic patients.
In the evaluation of complications, we compared incidences of intraoperative complications between diabetic patients and non-diabetic patients during cataract surgery.
Lastly, we compared postoperative outcomes between diabetic patients and non-diabetic patients after cataract surgery.
Our methodology included strict inclusion criteria, including no copathology, except amblyopia; no simultaneous surgical procedures, except intraocular injection; and clear ETDRS grading of retinopathy was required.
RESULTS
In examining preoperative risk factors, we found that epiretinal membranes (ERM), small pupil, and brunescent/ white cataract are more common in diabetics.
Our review of intraoperative complications found that posterior capsular rupture, dropped nuclear fragment, corneal edema, and overall complication rates were higher among diabetic patients.
In our examination of postoperative outcomes, we found that visual acuity, good vision (≤20/40), and pseudophakic cystoid macular edema (CME) were negatively associated with diabetes and degree of diabetic retinopathy.
The effect of preoperative diabetic macular edema (DME) on visual acuity and good vision was similar to the effect of having moderate non-proliferative diabetic retinopathy (NPDR).
As we evaluated outcomes, we looked at the difference in preoperative and postoperative visual acuity between the diabetic and non-diabetic patients.
Using logistic regression analysis for pre- and postop (four to 12 weeks) BCVA > logMAR 0.3 with 95% CI, we examined the chance of having poor vision postoperatively.
We examined the chance of having pseudophakic cystoid macular edema postoperatively, using logistic regression analysis for postop CME with 95% CI. We also wanted to determine if we could predict postoperative vision based on preoperative vision and diabetic status.
We utilized a linear regression model for age, preop DME, diabetic status, preop visual acuity, and postop visual acuity at four to 12 weeks with 95% CI.
There also are some limitations that we acknowledge, including retrospective design, missing short-term follow up data, and missing details of grading of cataract type/density. We found that diabetics are seeing worse, they are having poor vision and are developing more macular edema after surgery.
The worse their retinopathy, the worse their outcome. This study provides data to assist in the planning of cataract surgery and providing informed consent in diabetic patients.
It would be reasonable to recommend performing cataract extraction on diabetic patients early, before the development of significant retinopathy or vision decline.