Cataract Surgery & Dropless – Perioperative Treatments
Cataract surgery is the most commonly performed ocular surgery and one of the most frequently performed surgical procedures worldwide.
The vast majority of patients undergoing cataract surgery (99.5%) has a successful result with no serious adverse events and can expect improved distance visual acuity after surgery.
With presbyopia-correcting lenses, patients may achieve good uncorrected acuity at near and far.
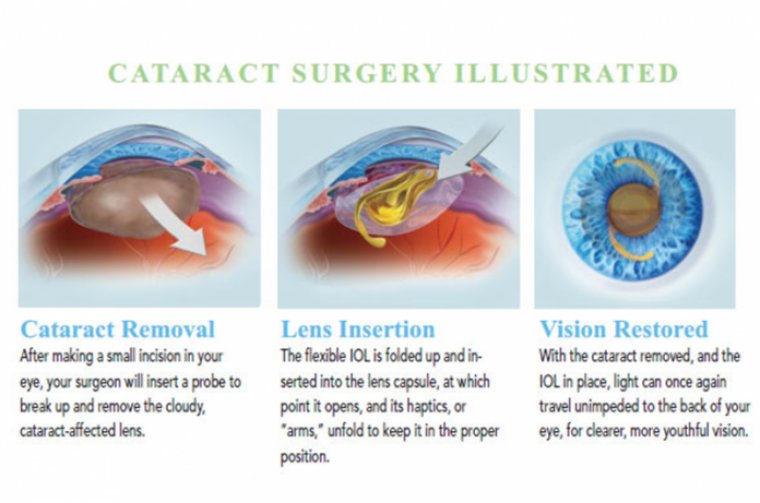
In the United States and most developed countries, smallincision, sutureless surgery is performed, using advanced ultrasound phacoemulsification and, in some cases, femtosecond laser technology.
A foldable intraocular lens is implanted after removal of the cataract. Recovery time is minimal, with most patients seeing well the first day after surgery, and final visual acuity is achieved within one month.
Risk reduction and the attainment of good outcomes depend in part on patient compliance with a postoperative regimen of eye drops.
Patients typically are instructed to instill topical antibiotic drops a few days before surgery and 1 to 4 times daily for 1 week or longer after the surgery for the prevention of endophthalmitis, a rare but devastating complication.
Endophthalmitis occurs in approximately 0.01% to 0.25% of eyes treated with povidone iodine scrub, depending on the practice patterns for other prophylactic measures.
Recent changes in regulation, insurance coverage pharma guidelines and patient expectations have created a pressure cooker in the perioperative cataract surgery medication space, resulting in a landscape filled with new opportunities.
The resulting alternatives to traditional pharmaceutical delivery over the last few years have helped create an increasingly nuanced approach to cataract surgery.
THE COSTS OF CHANGE
Most ophthalmologists agree that an antibiotic, steroid, NSAID medication or a combination of the three should be used throughout the postoperative period to assist the healing process.
Antibiotics are used as a prophylaxis measure to prevent endophthalmitis. Anti-inflammatory medication in the form of steroids or NSAIDs are used to control inflammation and as a prophylaxis for cystoid macular edema.
Traditionally, the medications were delivered with commercially branded eyedrop products.
Years ago, a provider could rely on insurance plans to cover the majority of a patient’s needs for perioperative eyedrop care and rely on samples provided by pharmaceutical companies to cover the rare patients lacking sufficient insurance coverage.
During those times, pharmaceutical companies even provided the “postoperative kit” as an added bonus to providers.
Times have changed, with rising drug costs combined with decreasing insurance plan coverage and high deductible plans resulting in postoperative drug costs that can exceed $650, which is often more than the professional fee to perform the surgery.
Furthermore, many patients are subject to a potential three-drop regimen with a complicated dosing schedule, resulting in poor compliance and frustration on behalf of both the patient and the provider trying to explain and ensure the medications are taken properly.
This complicated regimen coupled with potentially staggering costs have led many to wonder, “Do we need all these drops after cataract surgery?”
THE “NO-DROP” DREAM
There has been a recent push to pursue the dream of no-drop cataract surgery. Surgeons began to innovate the space with a compounded product of triamcinolone and moxifloxacin, which is delivered at the time of cataract surgery to help eliminate the need for postoperative drops.
Based on Medicare reimbursement laws, this medication must be purchased by the surgery center or hospital and included in the facility fee (patients cannot be charged out-of-pocket fees for medications delivered at the time of cataract surgery).
With that said, many centers have found it worthwhile to provide intraoperative medications, which typically results in greater patient goodwill and decreased staff time when dealing with pharmaceutical-related phone calls.
Intraoperative medications have proven successful in endophthalmitis prophylaxis, but this technique is not without trade-offs.
For instance, the technique requires a learning curve to surmount as the medication is delivered into the vitreous either through one of two approaches: a “trans-zonular” or a “pars-plana.”
The trans-zonular approach involves a cannula being passed through the zonules at the end of cataract surgery, while the pars plana approach uses an injection of medication delivered via a needle passed through the sclera.
Both approaches have their advantages and disadvantages and require proper surgical technique.
COMPOUNDING 101
Beyond the technical aspect of the drug delivery, there are also potential inflammation concerns secondary to the lack of NSAIDs present with the “dropless” technique.
With “dropless,” upwards of 10% of cases have an incidence of breakthrough inflammation requiring supplemental drops, as well as a potential of cystoid macular edema — both of which may require supplemental steroid and or NSAID eyedrop delivery.
Because of these risks, many surgeons have moved to an alternative approach through eye- drop reduction and simplification.
For example, Imprimis Pharmaceuticals has created a “less drops” product composed of prednisolone acetate, moxifloxacin and bromfenac, thus combining a steroid, NSAID and antibiotic medication into one bottle, allowing for the drastic reduction of drop medication.
Furthermore, a compounded medication can simplify the postoperative drop regimen and may reduce the patient cost to less than $100 total for the combined compounded medication.
Branded pharmaceutical companies have also worked to develop once-a-day dosing schedules to help simplify the post-operative period. For example, BromSite (Sun Ophthalmics) is available and typically dosed once per day around cataract surgery to help control inflammation and prevent CME.
Quality and safety concerns with compounding medications have arisen, though, so it is critical to ensure the medication is formulated properly with stringent quality controls.
The FDA has established a 503B standard that may help alleviate some compounding concerns, such that medications compounded in a 503B facility are held to many of the same baseline standards as commercial pharmaceutical companies.
Beyond potential safety considerations regarding the importance of proper sourcing from 503B level pharmacies, compounded drops are not without logistical challenges, especially since the dispensing process adds a layer of complexity on the clinic side.
Providing drop medications to patients requires a pharmaceutical dispensary license, which requires following a state’s dispensing guidelines to stay compliant. Furthermore, traditional compounding dispensing requires medication to be ordered on a patient-by-patient basis, thus resulting in some logistical complexity.
The new 503B guidelines have simplified this process by allowing clinics to bulk order without patient identification and dispense medication on an as-needed basis.
Furthermore, physicians find it reassuring to know that patients are getting their proper medications and have them in hand after surgery. With physician-dispensed pharmaceuticals, there is no doubt that patients have the medications that were ordered by the physician.
This is an improvement over the recent generic medication push. Compounded medications should not be confused with “generic” medications. Physicians order compounded meds and understand exactly where the medication is made and what it is made from. With generics that assurance does not exist.
In summary, if done properly in a well-managed system, many providers have found that dispensed compounded medication allows for a more pleasant patient experience by eliminating the frustrations that come with dealing with insurance reimbursement, generic substitution and commercial pharmacy call backs.
Using both the compounding drop approach and intraoperative medications, some surgeons have found they can provide simple comprehensive coverage.
By providing both intraoperative medications and postoperative drops, one has the potential to reduce the postoperative eyedrop requirement.
For example, many providers have utilized a technique in which they deliver medication intraoperatively along with a postoperative course of compounded triple medication drop at a one-time per day dosing schedule.
With this approach, the intraoperative dose covers the majority of antibiotic and inflammation prophylaxis, while the simplified postoperative drops help eliminate CME and breakthrough inflammation.
INTRAVITREAL: BENEFITS AND RISKS
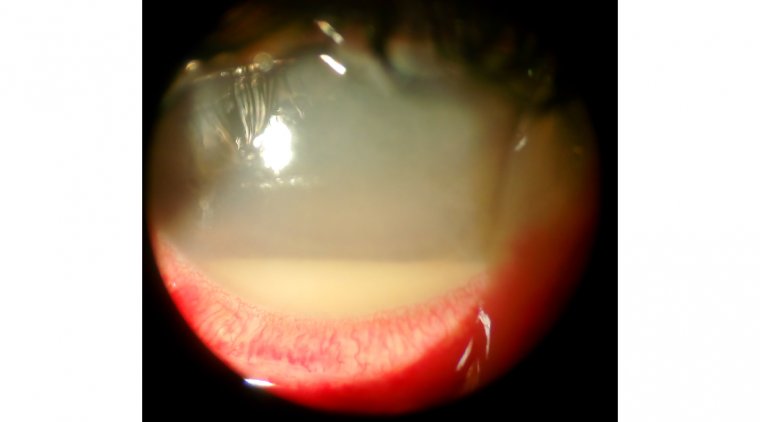
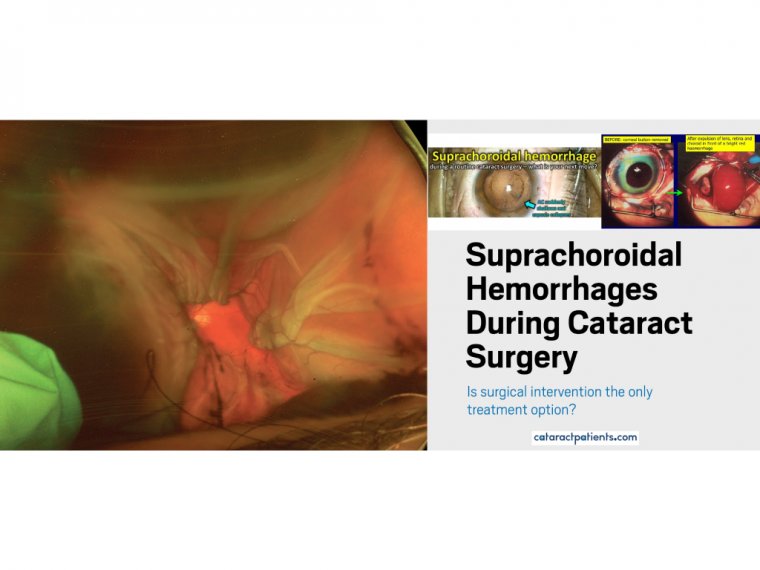
Other concerns have arisen from using intraocular medications at the time of surgery. For example, research has shown an association of occlusive retinal vasculitis with the administration of vancomycin inside the eye.
This association is rare, but it has some surgeons wondering if the benefit of intraocular vancomycin is outweighed by the potential risk. Another concern related to intravitreal medications has arisen after a series of acute retinal toxicity appeared related to compounded moxifloxacin.
It is believed that this localized outbreak of toxicity was related to improper formulation of the medication from a solitary compounding pharmacy.
There have been no reported toxicity events related to Imprimis’ proprietary Tri-Moxi formulation. Other pharmacies have attempted to recreate the Tri-Moxi medication that Imprimis initially pioneered, and there is a potential of improper formulation if steps and medication sources are not followed carefully.
PERIOPERATIVE INNOVATION
Other reasons to consider alternative approaches stem from a limited amount of financial resources. Until relatively recently, most insurance plans paid for the best available surgical techniques and whatever medication the physician felt was needed to achieve the best results.
Health care has transitioned into a functionally two-tiered system with out-of-pocket fees for “premium” technology.
Furthermore, many patients are currently forced to be on insurance plans with high out-of-pocket deductibles.
These facts are pressuring physicians and patients to ensure proper value is being delivered. With these out-of-pocket pressures and an actual and theoretical limit to what patients can spend, the pharmaceutical portion of cataract surgery is tapping into the same resources needed to pay both basic and upgraded options.
By allowing patients to shift dollars from expensive commercially available products, they may then apply those dollars to premium services or at the very least be able to afford basic cataract surgery through savings in alternative medication techniques and sources.
The pressures of cost, convenience and rising patient expectations have helped spark recent industry innovation in the perioperative drug space. Three notable examples are Omidria (Omeros, Inc), Dexycu (Eyepoint Pharmaceuticals) and Dextenza (Ocular Therapeutics).
Omeros was one of the first in the space with Omidria, an intraoperative medication composed of 1% phenylephrine and 0.3% ketorolac used for surgical pupil dilation and patient comfort.
Omidra is currently reimbursable via the “Transitional Pass-Through Status under the Hospital Outpatient Prospective Payment System (OPPS),” a Medicare fund designed to support innovation in outpatient surgery.
This funding pathway allows medications to be purchased on a pass-through status, thus avoiding increased expense for the patient, provider and facility.
The result is a billable fee that is added onto the surgical facility fee that is then utilized to purchase the Omidria, which is reimbursed by Medicare through the pass-through pathway.
Omidria has proven successful in maintaining a dilated pupil during surgery, and some providers wonder if the NSAID delivered during surgery may help alleviate the need for postoperative NSAID drops. Future studies will hopefully explore this and help prove or disprove the effect of such drops.
One of the most important aspects of Omidria is the pioneering aspect of its reimbursement pathway. The reimbursement was initially controversial, as an additional fee of more than $400 is added onto the facility fee to cover the cost of the Omidria medication.
However, providers began to realize that, for innovation to occur within the space, it is helpful for the Medicare program to contribute to such advancements through pass-through funding. Via this funding, the benefits of Omidria are realized by the patients, allowing for the financial support of this type of “start-up of company”.
Companies like Eyepoint and Ocular Therapeutics will also make use of the pass-through pathway. Both Dexycu and Dextenza provide steroid delivery that can aid postoperative healing. Both utilize the pass-through pathway, allowing for Medicare reimbursement and avoiding facility, physician and patient expense.
Dexycu is a proprietary suspension delivered into the anterior chamber resulting in a slow release of dexamethasone medication.
Similarly, Dextenza releases dexamethasone via plug placed in the lower punctum of the eyelid. Both may help eliminate the need for steroid drops in the postoperative period.
Patients will still need NSAIDs and antibiotic medications delivered either through drops and or via intraocular delivery at the time of surgery.
Unfortunately, recent health industry changes have challenged the sustainability of traditional pharmaceutical delivery methods. Thankfully, we as a field have adapted to the changing environment. Our flexibility has led to innovative approaches that have not only simplified the process but also allowed for increased cost savings, convenience, safety and efficacy for our patients.