Pre-operative IOP Hints After Cataract Surgery
The phenomenon of elevated IOP following cataract surgery has been documented since the 1950s. In 1976, a review of 630 cases of cataract extraction with lens implants concluded that elevated IOP was transient and benign.
Nearly all patients' pressures returned to baseline with or without treatment. Some individuals, however, may experience pain, corneal edema, glaucomatous nerve damage, or anterior ischemic optic neuropathy.
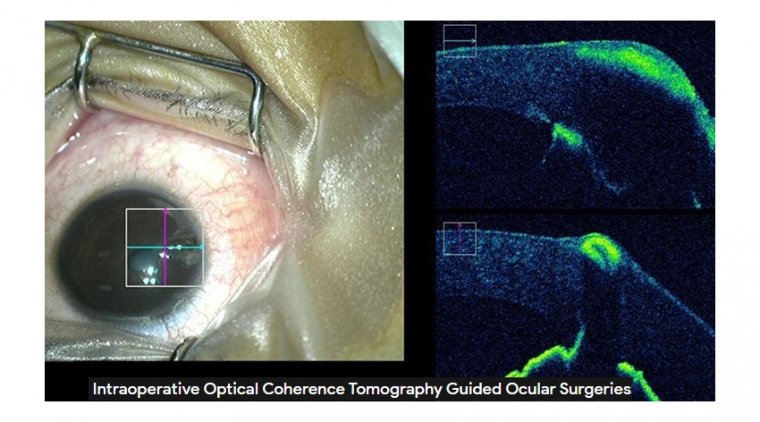
It is therefore important to continue monitoring the effect of new cataract surgical techniques on postoperative IOP as well as the impact of increased IOP on visual outcomes.
The concurrence of glaucoma and cataracts, coupled with the fact that the only known modifiable risk factor in glaucoma management is IOP, has heightened interest in the effect of cataract surgery on IOP.
The observation that IOP often decreases after cataract surgery was first published several decades ago. Many studies have since investigated this finding, and there are several extensive reviews of the subject.
Cataract surgery has been described as the single best glaucoma surgery due to its IOP-lowering effect.
Elevated IOP right after cataract surgery is the most frequent complication postoperatively and can lead to irreversible optic nerve damage and vision loss if not treated.
There remains a question, however, about the utility of using preoperative IOP as a predictor of IOP the day after cataract surgery in patients without glaucoma and ocular hypertension (OHT).
Elevated pressure and can lead to irreversible optic nerve damage, vision loss
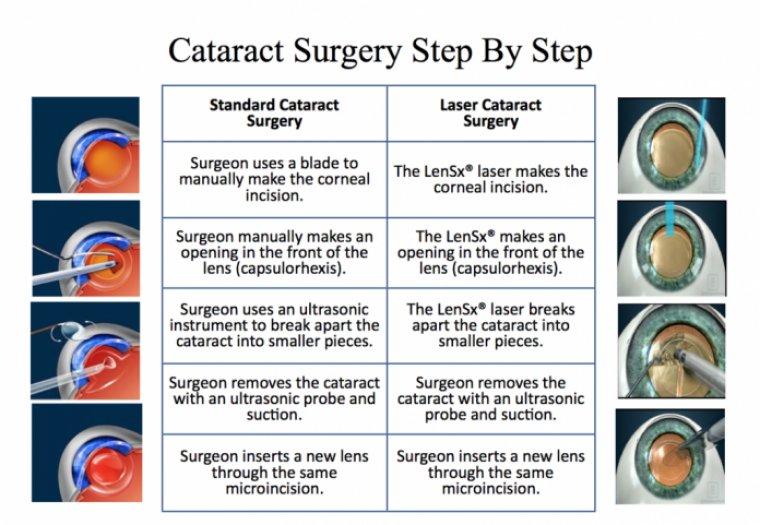
Although the long-term effect of cataract surgery is decreased IOP, a transient elevation of IOP is the most common complication in the days after cataract surgery and it can require treatment intervention, according to Madeline Hay, a third-year medical student at the Western University of Health Sciences, College of Osteopathic Medicine, Pomona, California.
Hay and her colleagues wanted to determine how preoperative IOP relates to the IOP on the first day after uncomplicated cataract surgery with IOL implantation in patients without glaucoma or OHT.
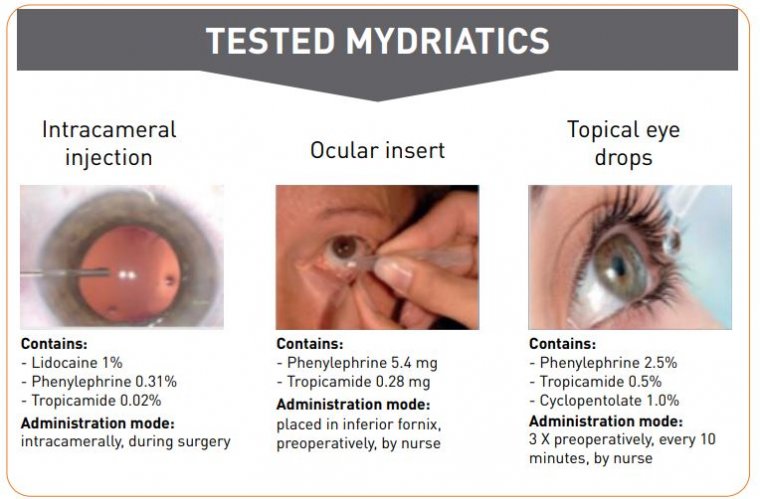
The investigators conducted a retrospective analysis of IOL implantation surgical data between January 1, 2016, and June 1, 2018, in patients older than 60 years who did not have glaucoma, OHT, pseudoexfoliation syndrome, or pigment dispersion syndrome; the study also excluded patients who had a history of IOP elevation in response to steroids, poorly dilating pupil, ocular trauma, or current use of IOP-lowering eye drops.
The IOP was measured preoperatively and postoperatively within 16 to 30 hours after surgery. RESULTS The investigators reported that 288 eyes were included; 56.9% of patients were women and the average patient age was 73.4 years. The average preoperative IOP was 15.98 mm Hg compared with the average IOP on day 1 postoperatively of 19.47 mm Hg.
Results indicated that the preoperative IOP was a significant (P < 0.0001) predictor of the IOP 1 day after surgery. Hay concluded that elevated preoperative IOP was associated with 1-day postoperative IOP elevations in patients without glaucoma or ocular hypertension following uncomplicated cataract surgery.
“This knowledge may help clinicians to identify patients at significantly increased risk for IOP-related complications,” she said. “Accordingly, this provides meaningful evidence in support of prophylactic preoperative treatment in high-risk patients to prevent loss of vision due to postoperative IOP elevations.”.