Cataracts With Unusual Corneas & Light-Adjustable IOLs
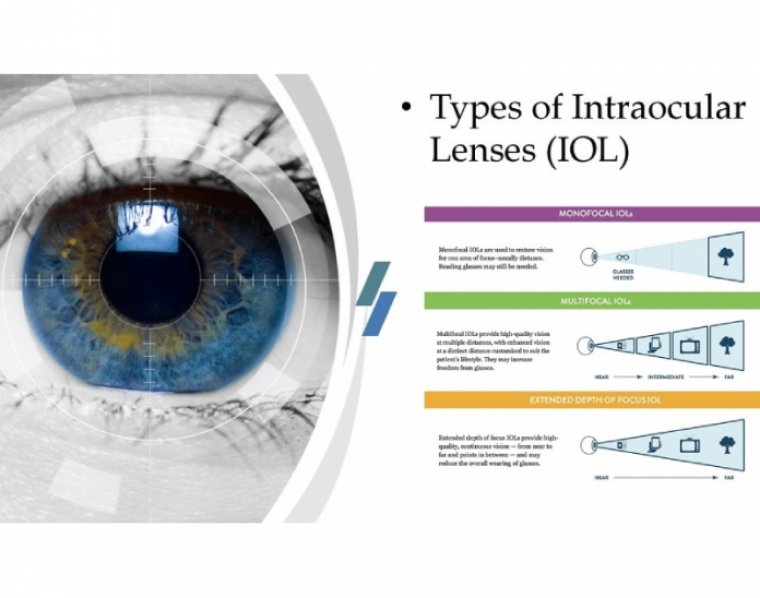
Light Adjustable Intraocular lens (LAL) are the only lens that allows post operative titrations in IOL power after the eye has healed and secured refractive stability post cataract surgery, facilitating customization an optimization of lens to achieve the desired vision.
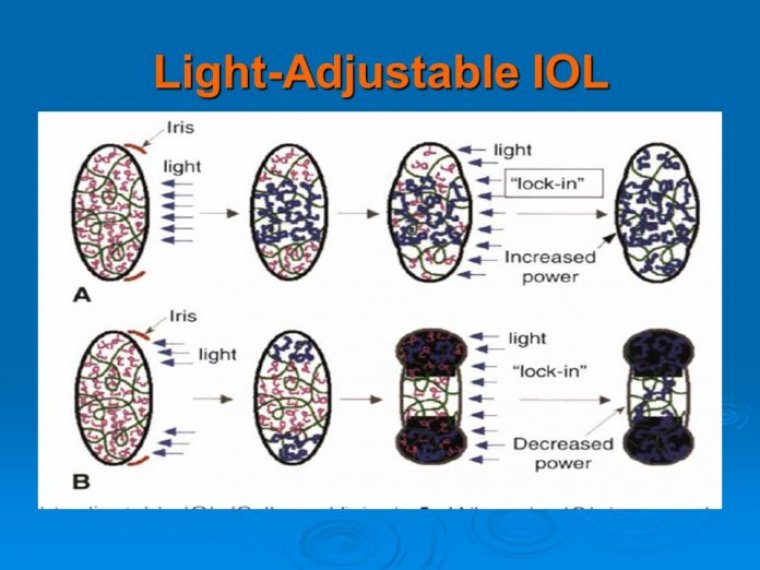
Light adjustability of the lens is based on the principles of photochemistry and diffusion. The LAL incorporates photosensitive molecules known as macromers embedded uniformly in a silicone matrix.
This polymerization creates a concentration gradient between the irradiated region and the rest of the optic.
Over a 12 hour period, the remaining unexposed macromers physically diffuse into the exposed area until there is no concentration gradient, causing an highly predictable change in the lens curvature and the refractive power change of the the lens.
Light treatments can simultaneously be targeted to perform spherical and cylindrical adjustments. As long as there are untreated macromers further adjustments to refine the corrections can be made by directing light to different areas of the lens.
When the adjustment process has been perfected to the satisfaction of the surgeon and the patient, the entire lens is exposed to the treatment light to polymerize all remaining macromers effectively locking them in place to prevent any further changes.
The light-adjustable lens (LAL; RxSight) may be a good solution for patients with cataracts who have unusual corneas, including patients with a history of radial keratotomy (RK).
These patients may otherwise have lessthan-optimal postsurgical refractive outcomes compared with patients with normal corneas, of whom from 80% to 90% are expected to achieve results within 0.5 D of the target refractions following cataract surgery.
The refractive outcomes in patients who have undergone RK are even more difficult to predict than those treated with LASIK or PRK. A recent study that found the best percentage within 0.50 D achieved in patients who had previously undergone RK was 69.2% in the short term.
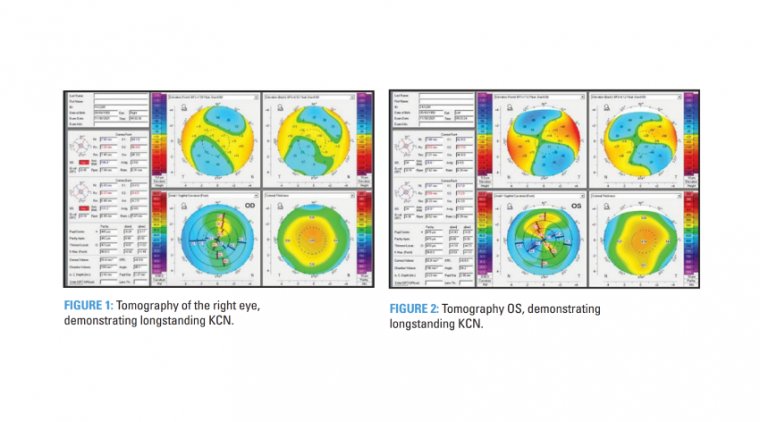
The difficulty in predicting outcomes in postRK cataract is a consequence of the small, irregular optical zone, irregular astigmatism, and an altered anterior/posterior ratio.
And despite useful tools such as intraoperative aberrometry, the ASCRS IOL calculator, and modern intraocular lens formulae, we still struggle to obtain consistent postoperative refractive results.
Another study looked at the percentage within 0.5 D after RK 2 or 3 months following cataract surgery and found that results achieved with the various refractive formulae ranged from 50% to 63.5% in patients who were within 0.5 D of the desired refraction.
THE LAL SOLUTION
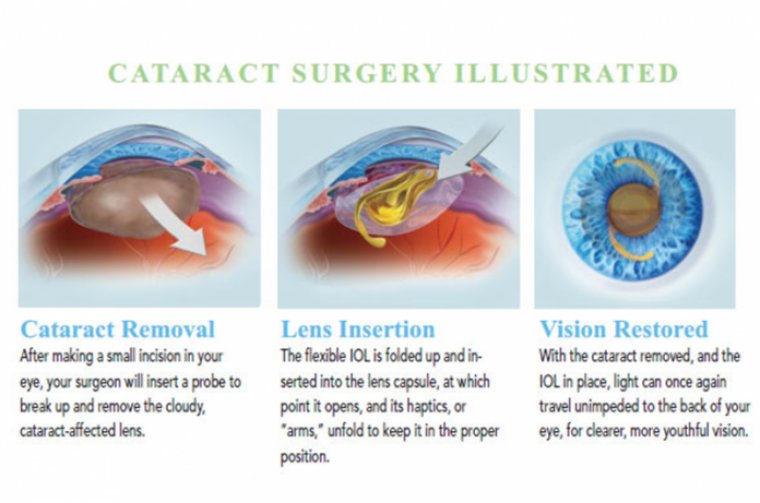
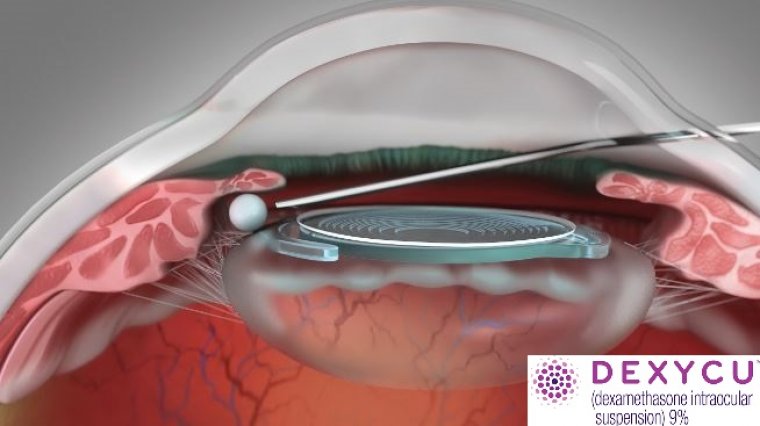
The LAL consists of a silicone optic with a special adjustable intraocular matrix supported by standard polymethyl methacrylate haptics. Following cataract surgery, a specific wavelength of light is shone on the optic to change its shape, thus changing its refractive power and helping to dial in the desired refraction.
This FDA-approved technology has been shown to work well in normal corneas, with the vast majority of eyes in the phase 3 FDA trial (92%) achieving 20/25 and almost 92% achieving results within 0.5 D of the target manifest refraction spherical equivalent.
Some colleagues wanted to examine how the LAL performed in post-RK corneas in both the short and long term. They performed a retrospective review of all patients (post RK) who received the LAL and identified 23 eyes in 14 patients.
The primary end points were the mean absolute error (MAE), the percentage of eyes within 0.5 D of target, and the mean refractive shift over time. All patients underwent cataract surgery bilaterally 1 week apart and returned for a series of light adjustments beginning 2 weeks after the second surgery.
Regarding the short-term results, the postoperative MAE before adjustment was 0.94 D and the percentage of eyes within 0.5 D before adjustment was 48%. This suggests that if the IOL were not adjustable, the results would be similar to the published data.
However, after adjustment, 95.7% of eyes were within 0.5 D and the MAE was 0.27 D. Only 1 eye did not get within 0.5 D of target.
The long-term results obtained at an average follow-up of 40 weeks indicated that the MAE was 0.43 D and the percentage of eyes within 0.5 D was 78.26%. These findings represented a decrease from the short-term results in both parameters, but the results were still good, Lehmann noted.
Additional analysis of the refractive shift in the long term showed an average shift in the spherical equivalent of –0.13 D and an absolute value shift in the spherical equivalent of 0.27 D. The average followup of 17 eyes was a mean of 50 weeks (range, 32-70). This translated to a shift that was not great over the long term. LAL worked well in patients who had undergone a previous RK. The MAE and percent within 0.5 D were better than the published data, and the long-term data also were good, although not as impressive as the short-term data.