Sedation in Cataract Surgery
Cataract surgery patients often wonder if they will be sedated for the procedure. Most cataract surgeries are performed under a local anesthetic.
This means that most patients are awake during their cataract surgery. This eliminates risks associated with general anesthesia and enables doctors to communicate with patients during the procedure.
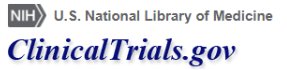
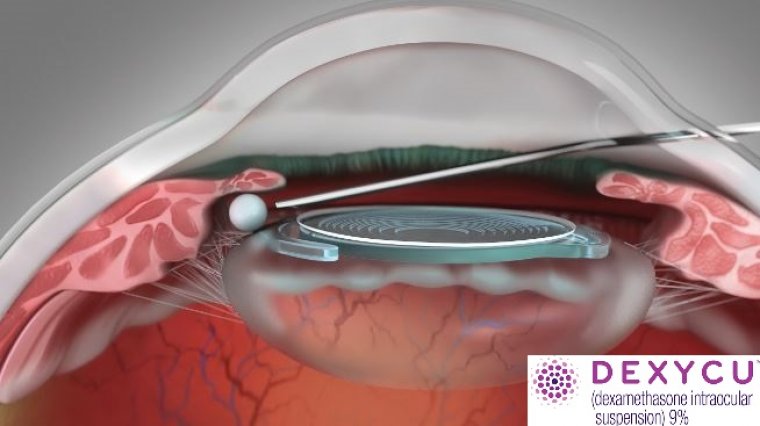
In a cataract surgery, the clouded lens of the eye is broken up and extracted. An intraocular lens (IOL) is then placed into the lens capsule as a replacement for the clouded lens. The procedure has variants, but generally, this is one of the most common ways that a cataract is surgically removed.
Cataract surgery is performed almost exclusively as an outpatient procedure. It usually involves the administration of a local anesthetic in addition to systemic sedation administered by an anesthesiologist or nurse anesthetist.
Surgeons' and anesthesiologists' preferences, as well as patient characteristics, are believed to influence the choice of anesthesia management for cataract surgery.
There are several strategies to provide the best mix of patient comfort, surgical outcomes (e.g., pain control, ease of performing surgery), and freedom from anesthesia-related complications (e.g., brainstem anesthesia, retrobulbar hemorrhage, globe perforation).
The choice of anaesthesia technique is influenced by the preferences of patients, anaesthetists and surgeons, the complexity of the procedure, resources and the healthcare delivery system.
There is no gold standard and management should be determined on an individual basis. Whatever the choice, the goals are to be safe, painless, efficient and effective.
Several approaches are used for cataract surgery, including: topical anaesthesia (eye drops); intraconal (retrobulbar); extraconal (peribulbar); and blunt-cannula (sub-Tenon's) blocks.
Topical anaesthesia involves the application of local anaesthetic to the surface of the globe and is associated with minimal discomfort during administration and the least complications. However, it does not block sensation arising from intra-ocular structures in the anterior segment.
Thus, intra-operative manipulation of the iris or stretching of the ciliary muscles may cause discomfort. Additional anaesthetic instilled into the anterior chamber (intracameral anaesthesia, usually with preservative-free lidocaine) improves patient comfort.
With steady incremental improvements throughout its evolution, cataract surgery has become one of the most frequently performed and successful surgical procedures worldwide.
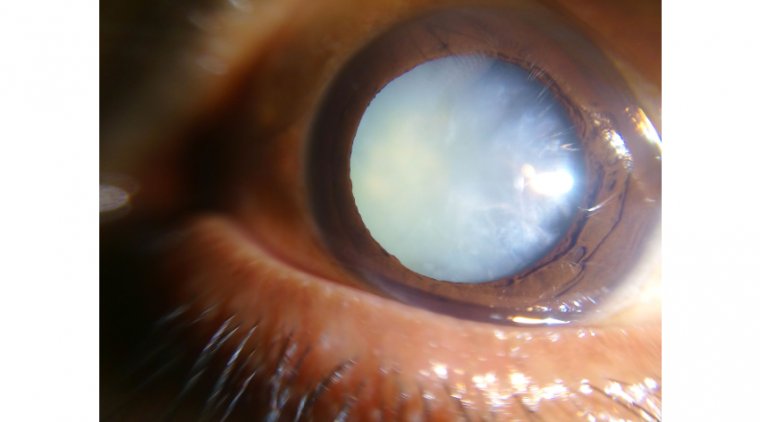
Despite this well-deserved track record, there remains a segment of the patient population that has reservations, and sometimes fears, about this procedure.
Having performed thousands of cataract surgeries, we find that patients are sometimes more stressed about sedation than about cataract removal and IOL implantation.
IV Option
Intravenous (IV) administration of anesthesia has traditionally been the method by which patients are sedated prior to cataract surgery.
Various IV agents, including midazolam, are used for this purpose. Midazolam, which is a benzodiazepine, has properties similar to an anxiolytic, a muscle relaxant, and an amnestic. These properties make it an excellent option for many but not all patients.
For instance, anxious patients who are administered IV benzodiazepines at cataract surgery might require higher doses during the procedure, which can result in oversedation.
This type of response can reduce the patient’s ability to follow simple commands and can affect the surgical outcome.
In addition, patients who receive too much sedation might nod off and awaken startled, which can compromise the surgical result. It is not uncommon for cataract patients to be nervous about IV administration.
Some patients are generally anxious, others have needle phobia, and there are those whose anatomy makes the needle stick challenging.
It may take more than 1 needle stick, for instance, if the patient has veins that are small or difficult to access, if patients are dehydrated, or if they have had multiple medical procedures.
Attempting sedation via the traditional IV method can be frustrating and painful for these patients and can slow down staff and patient flow.
Troche Approach
Patients often believe that IV sedation is the only option. Because of this, some delay cataract surgery, which can affect their quality of life as well as their safety.
For all these reasons, the movement to providing non-IV sedation is something we have been interested in for some time. We began offering MKO Melt (ImprimisRx) sedation in appropriate cataract surgery cases several years ago.
This method gives these patients the option of having surgery without the preoperative pain or anxiety related to IV catheter placement, while maintaining patient comfort.
The MKO Melt troche provides 3 mg midazolam, 25 mg ketamine, and 2 mg ondansetron, and delivers the medication via sublingual troche over a 2-minute release period.
The effects of conscious sedation are evident after 2 to 3 minutes, peak at about 15 minutes, and provide adequate sedation for up to 1 hour.
The combination of ketamine and midazolam offers a level of sedation that is efficient and effective for patient sedation and comfort. Ondansetron adds an antiemetic to the compound.
The troche has several advantages, including the following:
> It is nonopioid.
> It is easier for patients, and most of our patients prefer it.
> It is quicker for the nurse anesthetist to administer.
> It has a rapid, reliable onset.
> It lasts more than long enough to keep the patient comfortable before, during, and after a typical cataract procedure, as well as during lengthier cases such as those that include implantation of a MIGS device.
Appropriate Candidates
Our MKO-to-IV sedation ratio varies from as low as 50/50 to as high as 70% MKO/30% IV on a given surgery day depending on the patients scheduled.
We make the initial decision regarding which type of anesthesia will best suit each patient at the consultation. We base this on their demeanor and medical history, and revisit and confirm or revise that decision on the day of surgery.
We start under the assumption that every patient will be a troche candidate. Once they have been evaluated, we determine whether they would be better suited to IV sedation.
For instance, if the patient is overly anxious or tells us that they have severe claustrophobia, we will opt for IV so that we will have the option of administering additional medication during the procedure if necessary.
There have been times in which the patient needed more sedation than the troche provided, for example if the case were prolonged. On those infrequent occasions it was simple to start an IV.
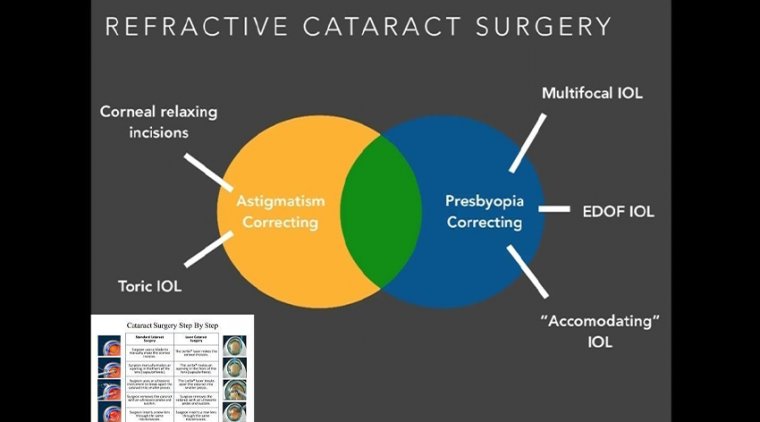
In IV sedation and MKO, the patient is aroused enough to communicate, which is necessary especially in cases where we are implanting an advanced technology IOL.
In these cases, the patient must fixate on the intraoperative aberrometry lights. This scenario represents another area where the MKO sedation method is beneficial because we have found that ketamine reduces photophobia and makes it easier for patients to focus on the lights and steady the eye.
Positive patient response and speedier patient throughput are just 2 anecdotal metrics that validate our use of the MKO Melt.
This practice is further supported by a recent clinical study that found that troche sedation is an effective and equivalent alternative to IV sedation in cataract surgery.
Jason Smith, CRNA, the lead author of the study, is affiliated with our practice and over the past several years has worked on seamlessly integrating sublingual sedation into our anesthesia armamentarium.
Now, his study provides evidence that patients were equally satisfied with the comfort level they experienced with MKO and IV sedation, and that is also what we find when we review our patient satisfaction surveys.
These surveys typically reveal that patients experiencing MKO were very relaxed and comfortable, and that if they had their second eye done at our practice under MKO after having their initial surgery done at a different practice under IV sedation, they preferred forgoing the needle stick.
Patients who had their initial eye done under IV sedation in our practice and their second eye under MKO also reported preferring the troche. Although patient comfort during cataract surgery is crucial, safety is paramount.
When investigators compared the effects of the MKO Melt with the effects of IV sedation on patients’ vital signs, they observed clinically and statistically significant improvements in preoperative and postoperative systolic blood pressure and postoperative heart rate in patients who received the MKO Melt.
They concluded that the MKO Melt was safe, effective, well tolerated, and a viable alternative to IV sedation.
Benefits and Bottom Lines
Another important benefit that we have found with troche sedation is that it provides a cost savings. It eliminates the need for IV tubing and IV solutions, and reduces personnel costs associated with IV insertion and removal.
Over the years we have striven to make cataract surgery a safer, simpler, and overall better experience for patients.
This has become even more of an imperative as refractive cataract surgery aims to satisfy the demands of younger, more active patients.
The MKO Melt represents a giant step forward in this evolution by providing patients with a relaxing and comfortable surgical experience, while eliminating the pain and angst associated with IV needles.