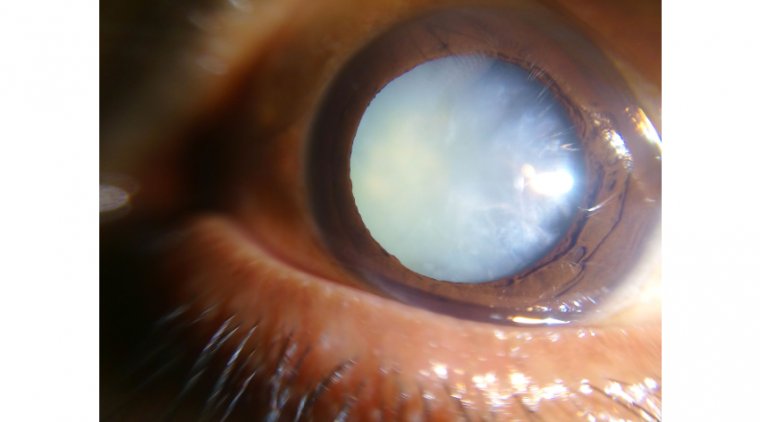
How To Deal With Dense Cataracts
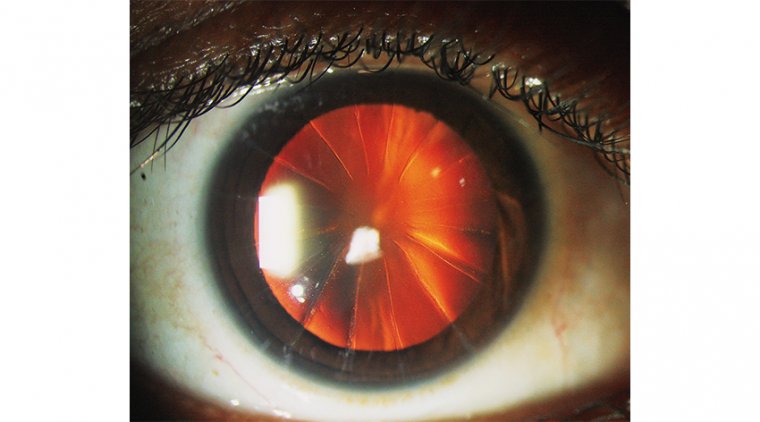
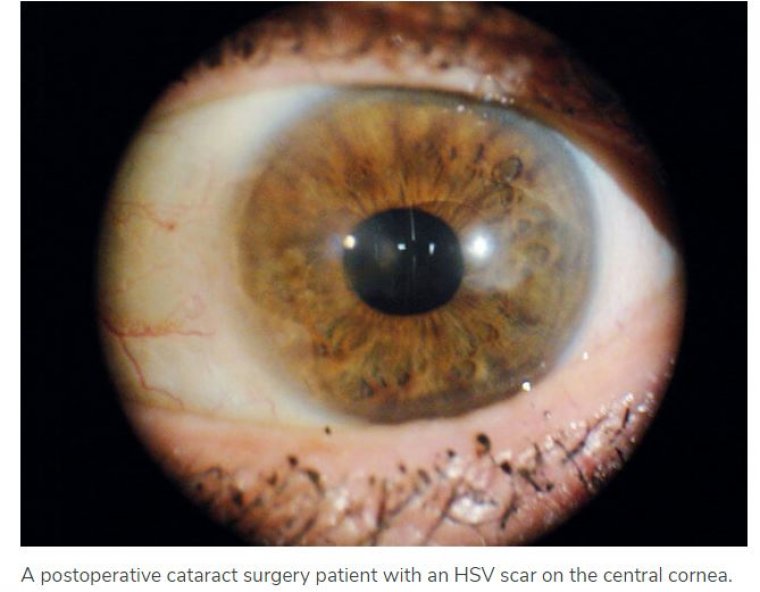
Removing hard cataracts can be difficult even for the most experienced cataract surgeons. Patients are typically older, with low visual acuity and coexisting ocular pathologies.
In this case, it is essential to get a detailed understanding of the patient's underlying conditions and prepare for possible challenges during the surgical procedure. Also, informing the patient about their condition is vital to managing expectations.
A dense cataract is, by its very nature, difficult to penetrate. This makes pre-op cataract evaluation a challenge. Both precise biometric measurement as well as screening for macular pathologies are key to avoid refractive surprises.
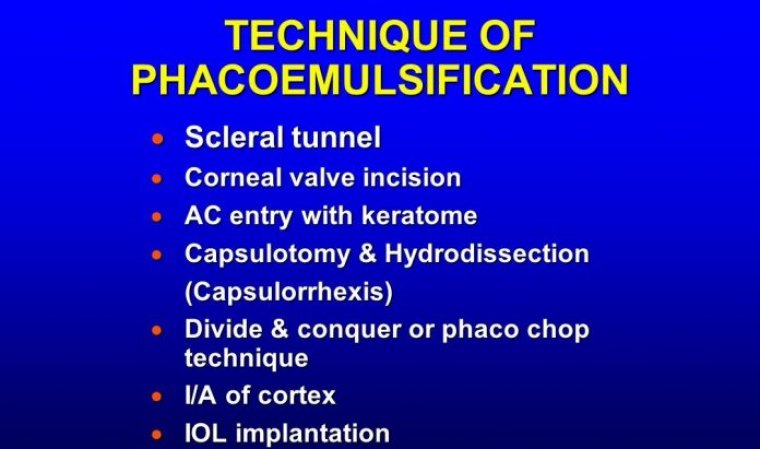
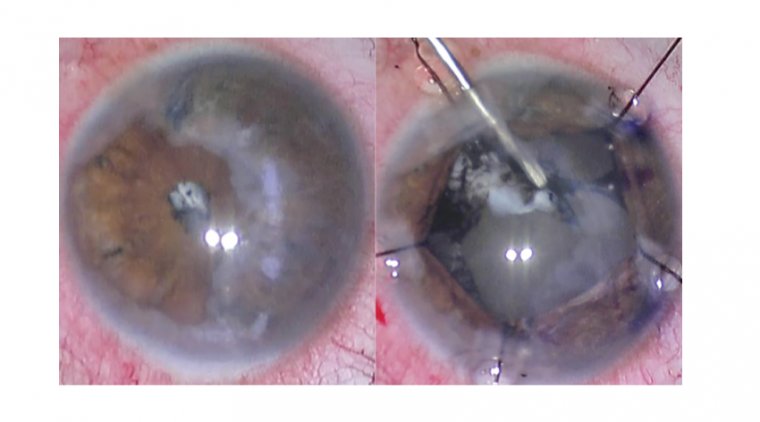
Lens fragmentation of a dense cataract requires a lot more phaco energy to emulsify the hard nucleus. More energy increases the risk of damage to corneal endothelial cells, which in turn can cause postoperative complications.
Extracting a dense nucleus is also associated with longer procedures, impacting practice efficiency in terms of time and costs.
REFRACTIVE CATARACT surgery has advanced at a monumental pace, bringing high patient expectations, more frequent procedures and higher disease severity.
Even with advanced IOLs and techniques, optimal clinical outcomes for patients depend largely on precision planning, which is facilitated by ocular biometer devices.
These instruments provide surgeons with valuable biometry and keratometry parameters that can be plugged into formulae for accurately calculating IOL power.
Pinpoint measurements have been shown to be essential for postoperative visual acuity, with even minor errors translating to notable postoperative refractive error.
CURRENT BIOMETRIC PARADIGM
Multiple options for performing biometric measurements are available, with varying technical modalities for determining the spectrum of essential parameters.
For example, the IOLMaster 500 (Carl Zeiss Meditec) utilizes partial coherence interferometry via a 780-nm infrared laser diode and lateral slit illumination for measuring anterior chamber parameters.
Another instrument, the Lenstar LS900 (Haag-Streit) employs optical low-coherence reflectometry via an 820-nm superluminescent diode to measure all axial parameters.
Although the precision of these older devices is well established in the literature, they fall short in performing axial calculations in more severely cataractous lenses.
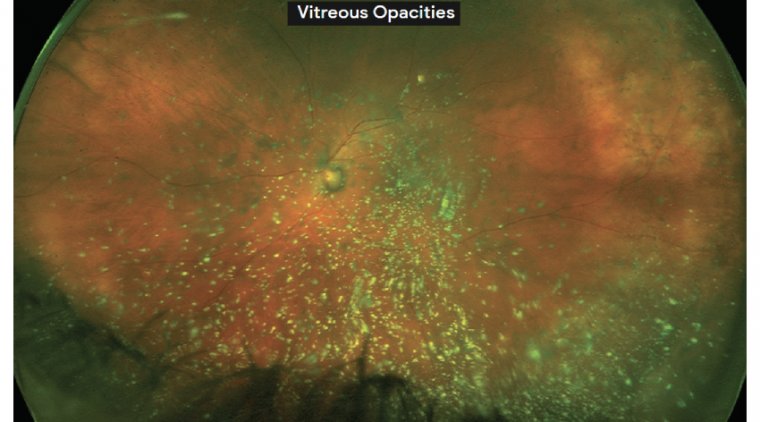
Both dense nuclear and posterior subcapsular cataracts are prone to light scattering, resulting in significant signal attenuation from the retina.
THE NEXT WAVE OF BIOMETRY
New biometers have been developed in an attempt to better serve patients with severe cases of cataractous disease. We now have several years of experience with one such biometer, the ARGOS (Movu Inc.).
Unlike older technology, this device utilizes a 1,060-nm wavelength and 20-nm swept-source technology to perform two-dimensional, full-eye optical coherence tomography (OCT).
This allows for comprehensive measurement of standard axial parameters, central corneal and lens thickness, pupil size, and aqueous humour depth.
In addition, a ring LED allows for keratometry. Furthermore, the device utilizes a safeguard system for patients unable to correctly fixate their vision during collection: a panoramic view of the eye facilitates alignment with the center of the pupil, mitigating initial measurement errors.
In addition, the system is designed to alert the user in the case of ongoing misalignment, allowing manual adjustment in particularly difficult cases.
But how does this technology benefit the patients previously mentioned, those with mature, dense, difficult-to-measure cataracts? In our experience the ARGOS far surpasses current modalities in measuring axial length in eyes with dense cataracts.
We have successfully performed measurements in many cases that would have been impossible with older devices.
Our experience includes successful and accurate measurements in patients with significant posterior subcapsular changes, latestage cortical changes and the highest severity of nuclear sclerosis.
With this biometer, axial length is truer to the absolute distance, as two-dimensional fulleye imaging allows for inclusion of characteristics that affect axial length but were previously unaccounted for, such as lens thickness.
The device also uses the appropriate refractive index (based on research and consensus) for the respective ocular elements, eliminating the need for nomograms that “correct” the axial length for significantly short or long eyes.
Additionally, the OCT employs a wide-scanning beam able to travel beyond the region of the cataract, so that retinal signals are no longer attenuated.
The increased wavelength facilitates deeper penetration of the cataract, removing a lot of the guesswork that went into determining accurate IOL power calculations for these patients. With this technology, we have personally measured axial length as long as 33.33 mm.