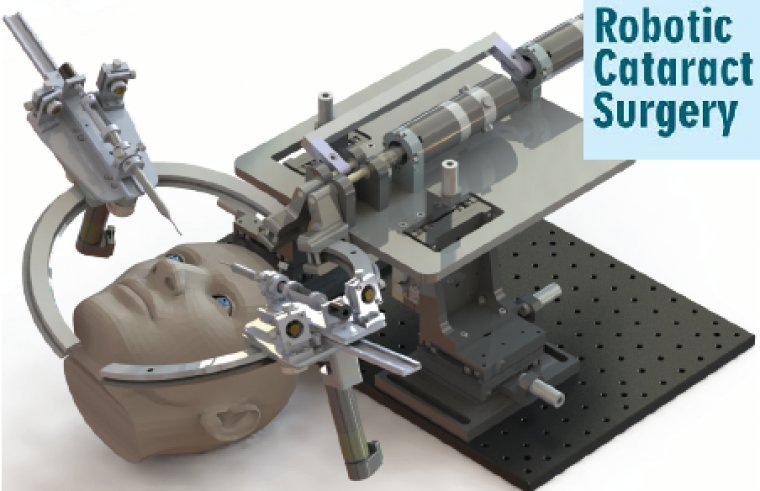
Robotic Cataract Surgery
The device uses a complete preoperative OCT scan to construct a model of the eye and plan surgery. During surgery, partial OCT scans are used to monitor where the automated instrument is in the eye, and direct it to lens and cortical material remaining in the capsule.
A surgeon monitors the operation and can over-ride the device if necessary. Potential advantages of automated surgery include more complete nucleus and cortex removal and reduced risk of capsule rupture by providing better visualisation, as well as eliminating physiological tremor in surgeons’ hands, and providing tactile feedback in semi-automated systems.
Robotic systems have been widely incorporated into many surgical applications because of their higher precision, greater maneuverability, and potential for improved sensing capabilities compared with manually performed surgical procedures.
The pace at which robotic systems have been integrated into ophthalmic surgery, however, has lagged behind that of other surgical fields. This difference can be attributed to the unique advantages of manual ophthalmic surgery, including direct visualization of the surgical workspace and unhindered maneuverability of intraocular instrumentation.
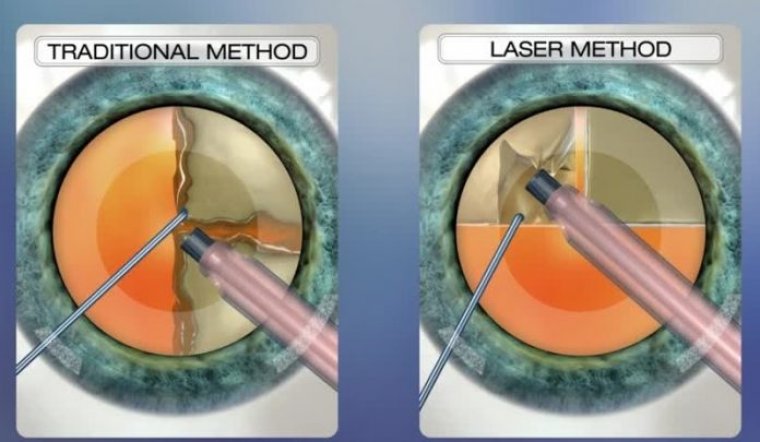
These advantages have eclipsed the apparent benefits of incorporating robotics into the ophthalmic surgical theater. Further, significant progress has already been made toward improving surgical outcomes through the incorporation of state-of-the-art digital microscopes, advanced fluidics control during phacoemulsification, and laser cataract surgery.
Nevertheless, manual surgical procedures are constrained by the physiologic limitations of the human surgeon.
Precise physical manipulation of intraocular tissue is hindered by inherent hand tremor, an inability to sense forces below those of human tactile perception, and a lack of sufficient depth perception to resolve microstructures or identify tissue planes.
These limitations do not hinder a robotic system to the same degree. This has inspired extensive research and development during the past 2 decades.
Here we highlight the beginnings of robotic surgery in ophthalmology, describe how robotic surgery is being used today, and discuss its future potential for cataract surgery.
BEGINNINGS
Since the early 1990s, dozens of robotic systems intended for intraocular surgical use, ranging from handheld to articulated robotic systems, have been prototyped and evaluated in research laboratories across the world.
The Micron, a fully actuated handheld robotic instrument developed by Carnegie Mellon and Johns Hopkins universities, has been shown to reduce hand tremor to provide a smooth, scaled motion during surgical procedures. A demonstrated application includes retinal vein cannulation on artificial vein models.
A research group at Vanderbilt University incorporated a B-mode OCT probe into a pair of microforceps to form a handheld surgical device that allows visualization of the membrane surface during epiretinal membrane–peeling operations.
The researchers showed that the tool-to-membrane distance could be known in real time from the OCT visualization and that this knowledge improved a surgeon’s performance during membrane peeling in ex vivo goat eyes.
In terms of articulated robotic systems, a research group at the Technical University of Munich demonstrated a mechanism small enough to be mounted to a patient’s head. This device was used to perform a range of intraocular procedures, including subretinal injection and deep anterior lamellar keratoplasty.
Recent work incorporates OCT-based needle segmentation techniques to expand the boundaries of autonomous surgical procedures.
To our knowledge, the only robotic system to be developed specifically for cataract surgery is the Intraocular Robotic Interventional and Surgical System (IRISS) from the University of California, Los Angeles.
Presented in 2013, the IRISS was the first robotic system to demonstrate simultaneous use of two surgical instruments, teleoperated capsulorhexis, and an entire cataract surgery on ex vivo pig eyes.
More recently, the IRISS was integrated with an OCT system to perform a range of autonomous surgical procedures, including partially automated lens extraction.
In that work, preoperative OCT scans were used to generate a lens-extraction trajectory, and intraoperative OCT scans localized around the tip of the I/A handpiece were displayed to the surgeon to enable real-time anatomical evaluation.
On an ex vivo pig eye model, posterior capsular rupture (PCR) was avoided in all trials, and nearly complete lens extraction was achieved with the IRISS.
CURRENT STATUS
To date, the Preceyes Surgical System (Preceyes) is the only robotic surgery system dedicated to ophthalmology to become commercially available. The system consists of a joystick-like motion controller used as an input by the surgeon and an instrument manipulator that mounts to the surgical instrument.
In 2018, the Preceyes was used to perform retinal membrane peeling and subretinal injection in humans. With this system, a high degree of tool-tip positional precision can be obtained, and virtual boundaries can be imposed to restrict unwanted movement and prevent iatrogenic retinal trauma. The Preceyes group continues to publish research results with their system, and at least three devices are currently being used in hospitals across Europe.