Cataract Surgery & IOL Psychology
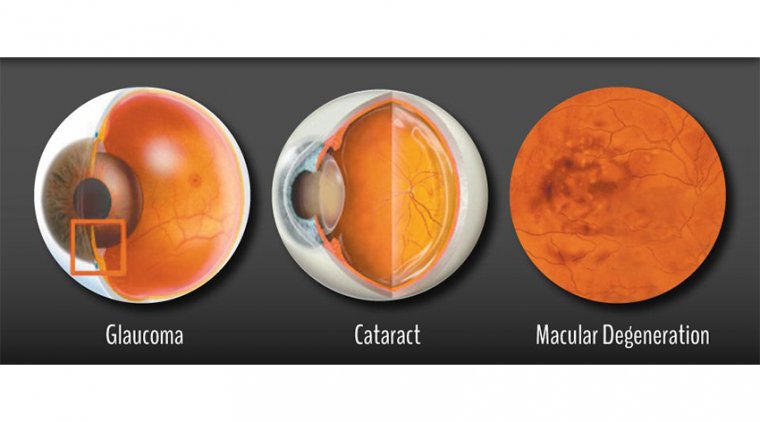
Eye surgery has been performed for over 1,000 years. Ancient Romans and Indians were performing ‘couching’ surgery on cataract-affected eyes as far back as the 5th century BC.
This surgery was extremely crude – the surgeon having to use a needle to slide cataracts away from the visual axis of the eye.
In more recent times, there has been a huge amount of innovation in the technology and practice of eye surgery.
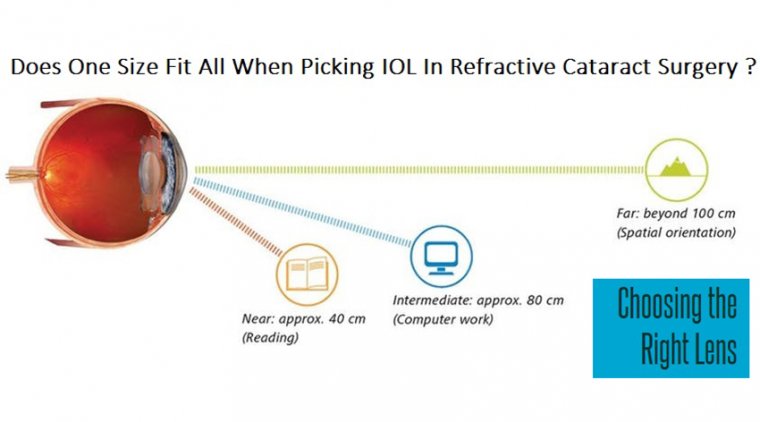
Based on the preoperative diagnosis including the corneal astigmatism, biometry measurement,IOL power calculation, presbyopia correcting IOLs’ indications and contraindications should be assessed for IOL selection strategy.
Surgical procedure should be technically optimized to achieve the best outcomes. Adequate management of both satisfied and unsatisfied patients will improve the benefit of current premium IOLs.
In recent years, premium intraocular lens options have expanded, including the previously elusive multifocal toric. Despite advances in technology and effective online biometry calculators, cataract surgeons’ conversion to mainstream use of premium lenses remains low, particularly for multifocals.
The reason is twofold, according to John Hovanesian, MD, a cataract, corneal and refractive surgeon in Laguna Hills, Calif.
First, surgeons must overcome the technical hurdle of choosing the correct lens for the patient to achieve the ideal refractive target. Second, they must sell a premium lens option to patients despite not being able to guarantee total freedom from spectacles.
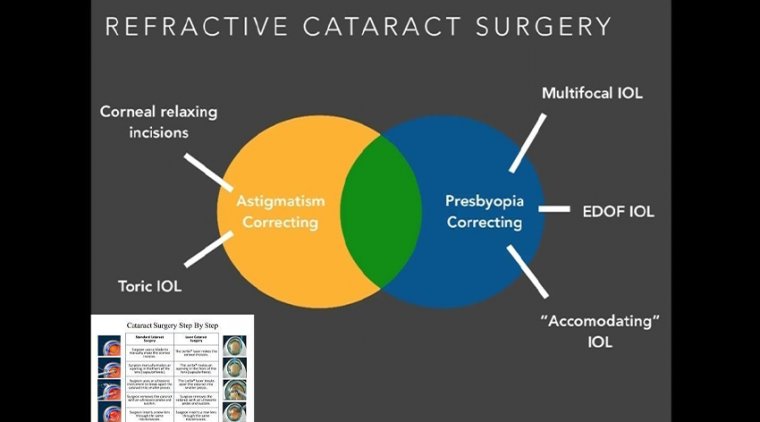
TORIC IOLS
Those interviewed agree that the maximum residual astigmatism after cataract surgery should be no more than 0.5 D to prevent reduced acuity, which decreases patient satisfaction.
John Ladas, MD, an ophthalmologist from Silver Spring, Md., says the key to addressing residual astigmatism postoperatively is a well-thoughtout plan. For low levels of astigmatism correction, this includes limbal relaxing incisions (LRI). Dr. Hovanesian offers patients LRI or arcuate keratotomy (AK) as a refractive upgrade and means of achieving the best possible vision.
In Perth, Australia, cataract and refractive surgeon Graham Barrett, MD, uses the Alcon AcrySof IQ Toric SN6AT2, which has an astigmatism correction of 0.68 D at the corneal plane to address low levels of astigmatism.
As a result, 80% of his cataract patients qualify for toric IOLs, he says (toric IOLs are covered by insurance in Australia). The prevalence of astigmatism in Dr. Barrett’s practice largely correlates with Warren Hill, MD’s, keratometry database of 6,000 U.S. patients, which shows that 72% of that population has greater than 0.5 D of astigmatism.
Levitz et al. showed that 94.7% of patients who received the SN6AT2 IOL achieved less than 0.5 D of cylinder postoperatively and 66.7% of patients had uncorrected distance acuities of 20/20 or better.
In this country, the lowest cylinder power Alcon IOL is the AcrySof IQ Toric SN6AT3, while the lowest cylinder of the Johnson & Johnson Vision IOLs are the Tecnis Toric ZCT150 and Tecnis Symfony Toric ZXT150.
All give a cylinder power of 1.03 D in the corneal plane. That leaves concomitant refractive surgery as the best and most likely option for low levels of astigmatism.
For cylinder amounts greater than 1.25 D, those interviewed say they are comfortable implanting toric IOLs.
Patient outcomes are generally very good, and the surgeons rarely need to rotate or exchange the IOL postoperatively — a rotation of fewer than 10 degrees changes the eye’s refractive error less than 0.5 D.
To improve refractive outcomes, they strongly recommend using one of the effective IOL calculator websites, such as IOLcalc.com or ascrs.org/barrett-toric-calculator.com , which incorporate posterior corneal astigmatism into the calculation.
The spherical equivalent postoperatively should be optimized to plano, says Dr. Ladas.
In 2016, Kessel et al. authored a study based on 13 randomized controlled trials. Seven hundred and seven eyes received toric IOLs and 706 eyes received nontoric IOLs (225 of which had LRIs).
The postoperative uncorrected distance visual acuity, spectacle independence and residual astigmatism were all better with toric IOLs than nontoric IOLs, even after LRI.
CLINICAL PEARLS FOR TORIC IOLS
For the best surgical results, “Remove all the viscoelastic postoperatively and leave the eye slightly soft,” Dr. Hovanesian says. “Do not overinflate it.
A distended capsular bag is more prone to rotation.” If rotation occurs, he suggests using the Berdahl & Hardten Toric IOL calculator (astigmatismfix.com ) to determine the required rotational correction.
Also, Dr. Barrett recommends procedural consistency to reduce surgically induced astigmatism following cataract extraction. “Enthusiasm has waned for small-incision surgery of values of less than 2 mm.”
He recommends an incision between 2.2 and 2.7 mm, ideally smaller than 2.4 mm, always located temporally, furthest from the visual axis. By using a consistent incision size and location, outcomes become more predictable.
ACCOMMODATIVE IOLS
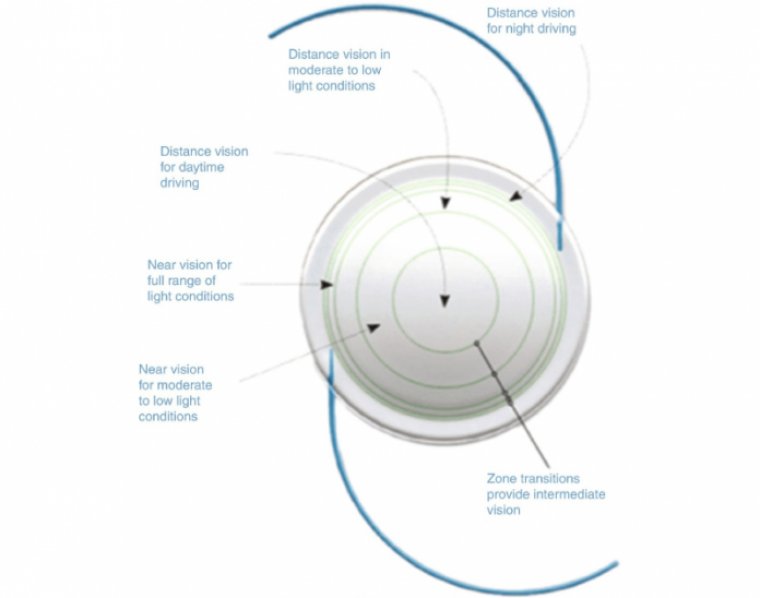
True restoration of accommodation would be the holy grail of pseudophakic presbyopia correction. The Crystalens AO (Bausch + Lomb) has haptics that are flexible, allowing the optical portion of the IOL to move slightly forward with contraction of the ciliary muscles, increasing the patient’s depth of focus.
Both Dr. Ladas and Dr. Hovanesian consider this lens for specific patients who want an accommodative option with spectacle independence for some near and intermediate tasks, but are not good candidates for multifocal IOLs.
Dr. Hovanesian has used the Crystalens AO in patients who have relative contraindications to multifocals, including post-radial keratotomy patients, those with aberrations from previous laser refractive surgery and cases of mild maculopathy.
In a study conducted by Sadoughi et al., 93% of Crystalens AO patients were more satisfied with near tasks and 71% were more spectacle independent after implantation, while patients with monofocal IOLs who were only 40% satisfied with near tasks and 24% spectacle independent after implantation.
However, only 64% of patients were satisfied with their vision for day and night driving, while every monofocal patient was satisfied with vision while driving. Also, accommodating IOL patients reported glare complaints more frequently than monofocal IOL patients, but the difference was not significant.
A meta-analysis comparing the functionality of accommodative IOLs to monofocal IOLs showed no clear evidence of near acuity improvement and an increase in posterior capsular opacification.
MULTIFOCAL IOLS
Both Drs. Barrett and Ladas prefer monovision with monofocal IOLs in both eyes over the use of multifocal IOLs.
They agree that an undercorrection of -1.25 D in the nondominant eye provides patients with effective intermediate vision without a significant compromise in depth perception and fewer issues with haloes and glare.
“Spectacle independence is not the most important outcome for many patients,” Dr. Barrett says. “Although some near vision is preferred, they do not want to compromise their quality of vision.”
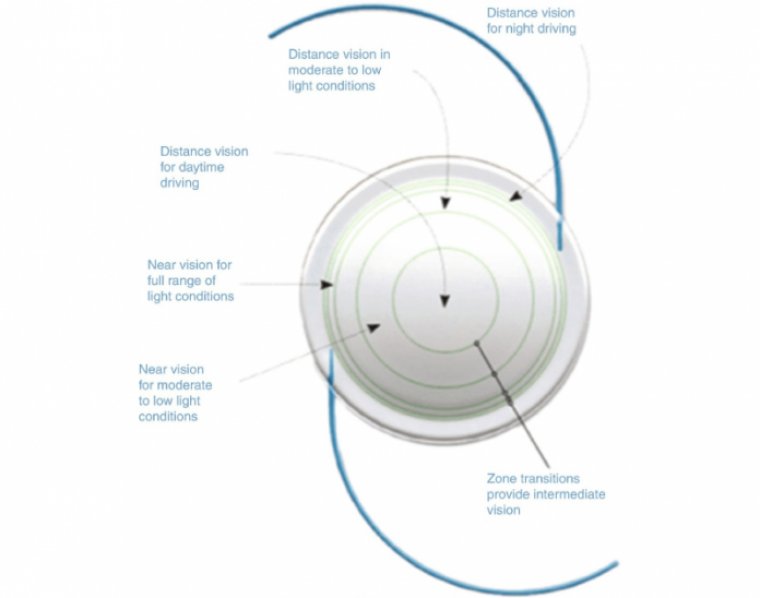
Dr. Hovanesian says he is comfortable with multifocals, particularly the improvements made in the last two years, which include the Johnson and Johnson Tecnis Symfony extended depth of focus (EDOF) IOL and the Alcon AcrySof IQ ReSTOR +2.50D spherical and toric IOLs.
His experience has been that lower near power multifocals provide better distance vision with less glare, haloes and dysphotopsia.
Dr. Hovanesian offers his patients “mini monovision” with either the ReSTOR +2.50 OU with a plano target refraction in the dominant eye and a -0.50 D target refraction in the nondominant eye, or a ReSTOR +2.50 in the dominant eye and a ReSTOR +3.00 in the nondominant eye.
Both results provide spectacle independence and good reading vision but offer less glare than a ReSTOR +3.00 OU.
In a study he presented at the 2017 ASCRS meeting, he compared 78 patients who received the ReSTOR +3.00 OU to 17 patients who received the ReSTOR +2.50 in the dominant eye and a ReSTOR +3.00 in the nondominant eye.
Both groups were equally satisfied and equally spectacle independent, but 56% of the +3.00 OU group noticed significant glare and haloes while these were only noticeable to 30% of the +2.50/+3.00 group.
At ASCRS in 2015, Dr. Hovanesian reported on another study involving 49 patients who had received multifocal IOLs five years earlier. 72% said they would not choose a lens with less glare if it meant they would require glasses for reading.
Dr. Hovanesian’s pearls for multifocal success are based largely on patient selection:
- Ocular factors such as dry eye disease and meibomian gland dysfunction are the enemy of accuracy. Assess and treat the tear film prior to surgery since persistent dry eyes degrade vision postoperatively.
- Corneal or retinal degenerations or dystrophies are relative contraindications.
- Patients with irregular astigmatism are poor candidates for multifocal toric IOLs because of unpredictable outcomes.
- Large pupils cause an increased risk of glare; small pupils make IOL insertion a problem.
- Capsulorhexis decentration is a risk factor for multifocal IOL decentration, which results in increased glare and decreased patient satisfaction. A decentration of approximately 0.75 mm or less is preferable and may be achieved using a femtosecond laser to make the capsulorhexis.
- Consider the patient’s lifestyle. Multifocals work well for those who want a range of vision with spectacle independence and are willing to compromise on distance acuity.
EXTRA TLC REQUIRED
According to Dr. Hovanesian, the main challenge in developing a successful premium IOL practice is not the technical aspects of surgical planning or execution.
“The harder challenge for most doctors is patient psychology, helping the patient understand what they need and what will make them happy, as well as how to best communicate to them what to expect and when.”
Dr. Hovanesian offered the following, “When considering multifocal IOLs, set proper expectations. Patients who expect surgical perfection have a high probability of being dissatisfied with multifocal IOLs.
Those who can’t understand the risks of aberrations, neuroadaptation to glare and potential for occasional spectacle use are also poor candidates.”
Extensive, unhurried discussions with patients are key to success with any sort of premium IOL, agree he and Dr. Ladas.
“The decisions we make together with our patients on refractive cataract surgery will affect them for the rest of his or her life,” Dr. Hovanesian says.
“Nothing builds trust and a satisfied practice of patients more than spending time to understand and be understood. The extra time it takes is the best investment we can make for our patients.”
Dr. Ladas concurs. It is critical to factor time into the practice’s schedule for such discussions. Dr. Ladas believes this courting process can be done efficiently — provided the surgeon has an effective system, forms and staff in place.
Talk with colleagues who have made a success of premium IOLs about how they handle such issues. “We do allocate specific time slots for patients that need or may want additional counseling” beyond the initial consultation, Dr. Ladas says.
SUCCESS IS A PROCESS, NOT AN EVENT
William F. Wiley, MD, from Cleveland, Ohio, agrees that patient education and expectation management is the key to successful outcomes, particularly when using multifocal IOLs. “It is rare to regret not doing a multifocal, but you do occasionally regret that you have implanted one.”
He has patients sign a consent form, indicating that the patient chooses whether they will use glasses postoperatively for distance or near, opting out of good vision, versus a premium IOL.
“Twenty years ago, when the lens became foggy, patients had cataract surgery and wore glasses, if they were lucky they would be less dependent on them. Now cataract patients are younger, more demanding, active and have higher expectations of freedom from glasses.”
Meeting these expectations requires more patient preparation time, and to achieve this Dr. Wiley has implemented the following system:
- Educate referring optometrists and provide them with literature to give patients. They already have longstanding relationships with their patients, including an element of trust.
- Mail information on premium IOL options to patients prior to the IOL consultation.
- Offer standing seminar dates once or twice a month at a community center or optometry office to educate prospective patients on outcomes, goals and lifestyle.
- Surgiorithm is an online survey tool that educates patients through video to determine their expectations, motivation and goals of cataract surgery. The surgeon receives a detailed report card.
- The patient is counseled by staff immediately prior to the surgical consultation.
- During the consultation, the surgeon examines the patient’s eyes and chooses the option that achieves the patient’s expectations based on the previous points. This takes only a few minutes because the patient is prepared.
- The scheduler/counselor answers any final questions.
COLLABORATION + INNOVATION = SUCCESS
Should the results fall short of the patient’s expectations in spite of all the extra time and attention, “This is where we really separate great physicians from capable technicians,” Dr. Hovanesian says.
“Great physicians always take the side of their patients, working to find the best answers and solutions until patients are happy.”
A concerned, collaborative approach tends to convince patients that the surgeon really is on their side, pre-empting any resentment. “Most patients understand and are grateful,” he explains.
Dr. Ladas describes achieving proficiency and success with premium IOLs as an ongoing process. “It occurs over years of listening to patients’ desires for a particular refractive result as well as their postoperative visual function with any type of lens … monofocal, monovision, premium.”
The cataract surgeon must become skilled, confident and proficient enough to truly believe they can deliver the refractive success that a premium lens can offer.