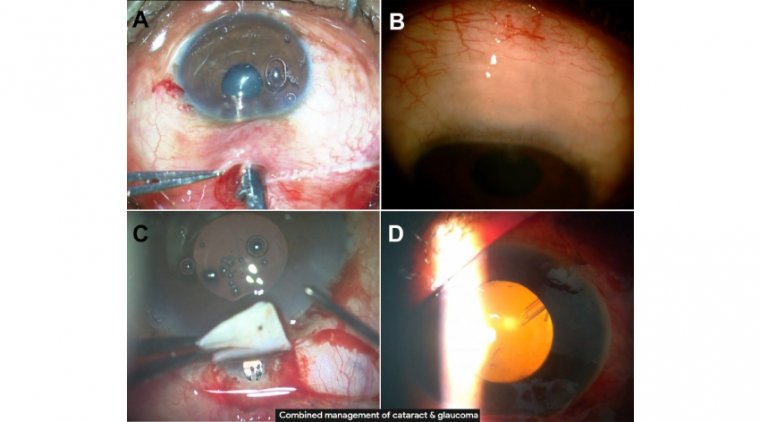
Techniques for Combined Cataract and Filtering Glaucoma Surgery
The decision for a combined procedure may be initiated by a need for cataract surgery or by a need for a filtration procedure.
In the presence of glaucoma, a filtration procedure at the time of cataract surgery can allow for better IOP control if cataract surgery alone is not likely to adequately decrease the pressure.
If a filter is required, it can be upsetting for a patient to have to undergo a second procedure. Careful examination of the lens and a combined procedure can spare the patient a second procedure, not to mention that a later cataract surgery could jeopardize filtration.
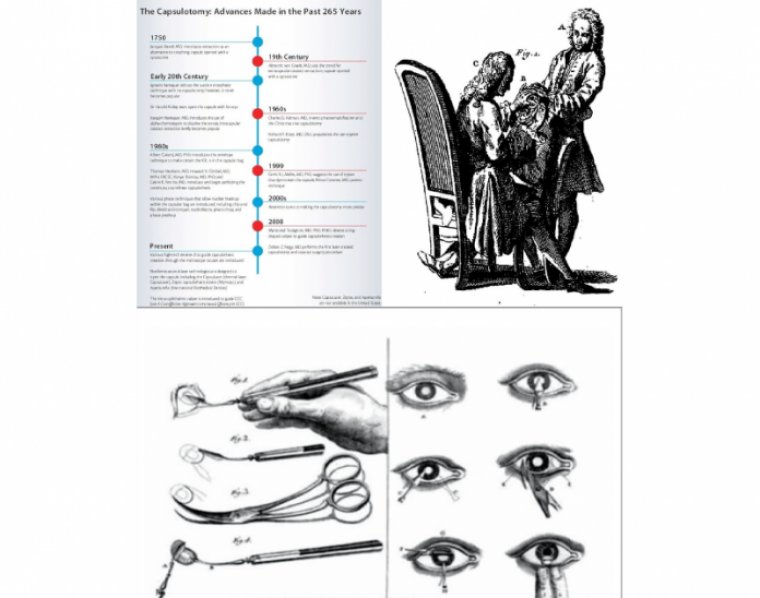
Cataract and glaucoma are the leading causes of blindness worldwide. The prevalence of both diseases is increasing with aging population. Techniques for cataract surgery have undergone significant refinements with excellent visual outcomes.
The goal of glaucoma surgery is to lower intraocular pressure to prevent or slow down the progression of optic nerve damage and associated visual field loss.
Although many patients present with these concomitant diseases, there is no general consensus on surgical management of coexisting cataract in patients with glaucoma.
The surgeon has to decide which approach may be best suited for a particular patient, combined surgery or staged (sequential) surgeries, depending on the patient’s severity of glaucoma and visual compromise from a cataract.
This brief review will discuss indications, surgical techniques, and outcomes of various types of combined cataract and glaucoma surgery.
Glaucoma is the second leading cause of preventable blindness, with an estimated 57.5 million people worldwide affected by primary openangle glaucoma (POAG).
Although we do not have enough glaucoma specialists to handle the sheer volume of glaucoma cases, the evolution of therapies allows cataract surgeons to take on a role in managing glaucoma and help fill in the gaps.
An increasing number of minimally invasive glaucoma surgeries (MIGS) can be performed during cataract surgery or on their own, with preparation and follow-up care that fit more easily into a comprehensive practice’s workflow than more invasive, traditional glaucoma procedures such as trabeculectomy and tube shunts.
When I came out of my training in cornea, there was a line in the sand: cornea specialists did not perform glaucoma procedures, and glaucoma specialists did not perform corneal procedures. I resisted doing any form of glaucoma surgery for a long time because of that formative culture.
Then one day, a friend said to me, “By not offering these patients a minimally invasive procedure that can help with their glaucoma while you’re doing their cataracts, you’re actually doing them a disservice.
If you asked them, they’d probably be all for it.” That resonated with me, and I decided to learn more about and train to perform MIGS.
We started with iStent (Glaukos), which had no effect on the outcomes of cataract surgery but resulted in a significant improvement in patients’ pressure and quality of life.
It grew from there, and now I do many MIGS procedures during and outside of cataract surgery.
About 20% of our cataract patients also have glaucoma, and about half of them elect to have a MIGS procedure at the time of surgery.
BENEFITS
Great visual outcomes
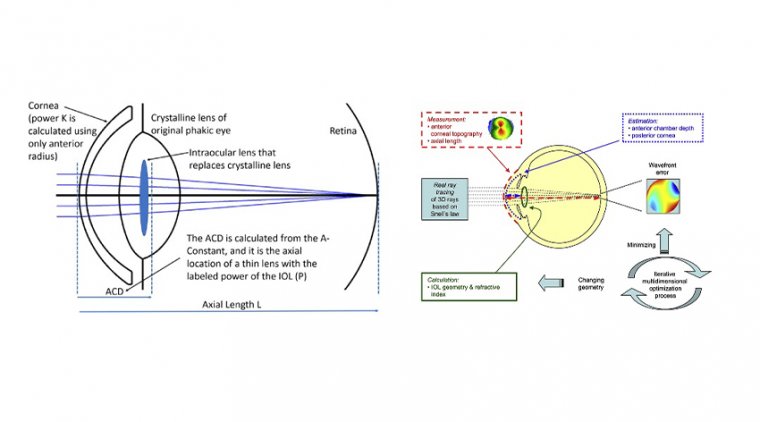
As cataract surgeons, we continuously hone our techniques to achieve the best visual outcomes.
When we heard about MIGS designed to be implanted during surgery, there was concern that we could compromise those outcomes, particularly because traditional filtering procedures may change the axis and magnitude of astigmatism.
Now we know that’s not the case. Visual outcomes for cataract surgery with iStent, Hydrus (Ivantis) or Omni (Sight Sciences) are the same as cataract surgery alone, even with premium lenses like torics or multifocals.
The XEN Gel Stent (Allergan), which is a subconjunctival procedure, has a much more posterior and low-lying bleb, so it also does not change the patient’s astigmatism or otherwise affect visual outcomes.
Decreased Medication Burden
After performing cataract surgery and a filtration procedure, patients can also reduce or eliminate the need to use topical medications. Lifting that burden at the same time as improving vision is an enormous benefit to a patient’s quality of life.
The precise difference depends on the severity of glaucoma, the number of medications they were on before surgery and the filtering procedure we perform. Even if a patient still needs one medication, pressures will be better controlled on medication than they were before surgery.
The importance of alleviating a glaucoma patient’s medication burden cannot be overstated. Several factors discourage compliance with glaucoma drops. Patients who must use topical medications every day will sometimes forget or delay getting their refills.
With glaucoma, that means pressures may not be reliably under control. Beyond inconvenience and forgetfulness, the medications can be expensive, so patients might weigh essential eyedrops against other necessary purchases.
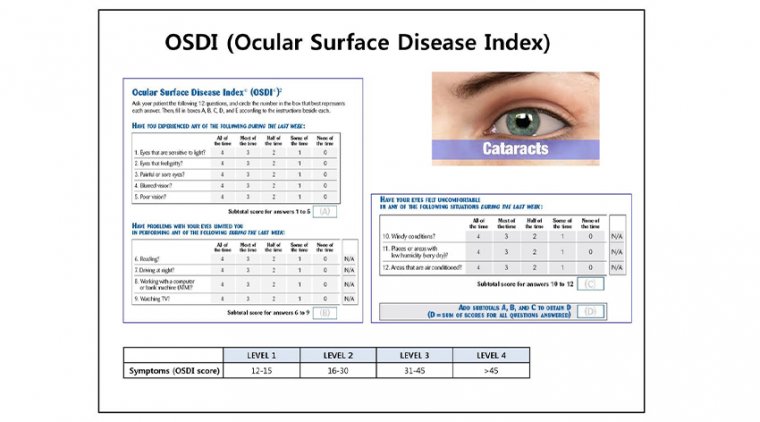
Topical glaucoma medications also have side effects. Although generally well tolerated, long-term glaucoma drops use can take a toll on the ocular surface or cause allergic reactions, particularly with multiple medications.
Another problem caused by longterm medication use is that ocular surface disease has been initiated or exacerbated by the drops and BAK preservative.
In our experience, it’s common to see patients on multiple drops with low tear breakup time (TBUT), high scores on dry eye questionnaires, and signs of meibomian gland dysfunction.
Their ocular surface is irritated, yet they must continue to use their drops and increase the BAK load to control their condition. After cataract surgery with a filtering procedure, patients often no longer need topical medications.
A patient who was using three drops might need only one. With little or no BAK load, I see their ocular surface continue to improve over time. Their dry eye scores get lower, TBUT increases and the clinical appearance of their meibomian glands improves.
Their eyes are more comfortable and show less injection. Patient relief You know how patients react when they’re happy with cataract surgery? Add to that happiness that comes from gaining their freedom from medications and side effects.
Take a patient who has had the responsibility of daily use of dorzolamide/timolol, brimonidine and latanoprost for years at significant cost, inconvenience and discomfort. Remove that inconvenience, cost and discomfort, and that patient is thrilled.
Their cataracts are gone, and so are the three bottles of drops. I think these patients are even happier than my premium lens patients who can get out of eyeglasses, which also results in word of mouth referrals.
GETTING STARTED
The learning process
Filtration procedures are very straightforward, and cornea experts and comprehensive ophthalmologists can be through the learning curve and start doing the procedures within a short time.
When my friend inspired me to do these procedures, I did some wet labs with iStent and began performing the procedures on patients soon after. You might also try learning from a colleague or asking a rep to connect you with someone in your area.
Differences Among Procedures
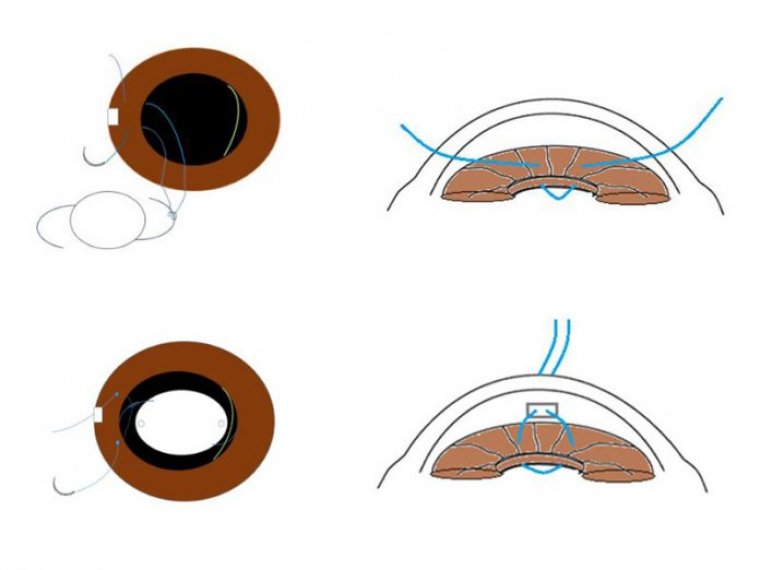
iStent and Hydrus are approved for use during cataract surgery only, while Omni and XEN can be used during surgery or as standalone procedures. The most important distinction between the devices, however, is their location.
Hydrus and iStent are stents placed in the trabecular meshwork, and the Omni is a microcatheter threaded through the trabecular meshwork to perform canaloplasty/trabeculotomy. All three can be done through the same incision used for cataract surgery.
The procedures can be done before or after the cataract, depending on the surgeon’s preference. The meshwork procedures require us to become good at intraoperative gonioscopy, which allows us to visualize the meshwork and carefully place the stent.
They all have their nuances. Some people may feel a little uncertain threading the Hydrus into the canal, while others may feel uncomfortable threading the microcatheter through the canal of Schlemm with the Omni.
It might take 10 cases or so to become proficient. The XEN is placed subconjunctivally like a tube shunt, but the procedure can be less complex. Many videos are online that provide tips to help with proficiency with XEN. I like to mark the stent with a marking pen prior to insertion.
This allows the stent to be better visualized in the subconjunctival space. About one in six of my XEN patients needs bleb needling. I had never done a bleb revision before and I was not looking forward to it, but I realized it is really not that challenging.
Choosing a procedure Learning curves vary based on the device and on your facility with gonioscopy. But, once you learn one procedure, the others are easier. Once you’ve mastered a few MIGS procedures, the choice of trabecular meshwork procedure is based on your preference.
We’ve talked with colleagues about which is best, and we all have different opinions based on what works best in our hands. I tend to choose the Omni and XEN for most circumstances.
XEN lowers pressure more than the meshwork devices, so while the candidate profile is the same for meshwork devices, we try to treat more advanced cases with XEN.
Recovery is identical to cataract alone for meshwork procedures, but XEN can cause some hypotony, and patients sometimes get a temporary choroidal detachment. As a result, I handle postoperative follow-up rather than sending patients back to the referring optometrist.
HEALTHY FOR THE PRACTICE, TOO
In the beginning, I only did MIGS procedures during cataract surgery, but as I became more comfortable with them and saw how good the outcomes were, I became more aggressive about recommending it for patients taking glaucoma medications.
I now do Omni and XEN outside of cataract surgery. I do a MIGS procedure in about 10% of my cataract cases, so the additional reimbursements are significant.
We also refer fewer patients to glaucoma experts — I probably refer patients once every other month for glaucoma procedures that are outside my offerings.
Still, the patients are the ones who truly benefit, with better control of their pressure and less dependence on topical medications. They’re now some of the happiest patients in the practice, and that’s really what it’s all about.