ASCRS Says Advocacy Work Leads to Victory for Cataract Patients, Surgeons
FAIRFAX, Va.—For the past year, the American Society of Cataract and Refractive Surgery (ASCRS) has been advocating on behalf of its members and cataract surgery patients to remove a policy put in place by Aetna that required preauthorization for cataract surgery.
ASCRS has now announced that as a direct result of its advocacy, with collaboration from the American Academy of Ophthalmology (AAO) and the grassroots efforts of its members, Aetna is dropping this policy.
Aetna no longer requires prior authorization for cataract surgery, except for Medicare Advantage (MA) beneficiaries in Florida and Georgia, a policy change that was effective July 1, ASCRS said in its announcement.
“As president of ASCRS, I'm thrilled about the work that was done over the past year by ASCRS and AAO that led to Aetna dropping its prior authorization policy for cataract surgery. As Richard Hoffman, MD, said last year, 'The best two people qualified to determine if cataract surgery is necessary are the patient and their ophthalmologist.'
I could not agree more and am pleased that right has been restored,” ASCRS president Douglas Rhee, MD, said.
“I'd like to personally thank the members of the ASCRS government relations committee, ASCRS government relations staff, and the members who personally reached out to Aetna for their tireless efforts advocating to maintain access to vision-restoring care for our patients.”
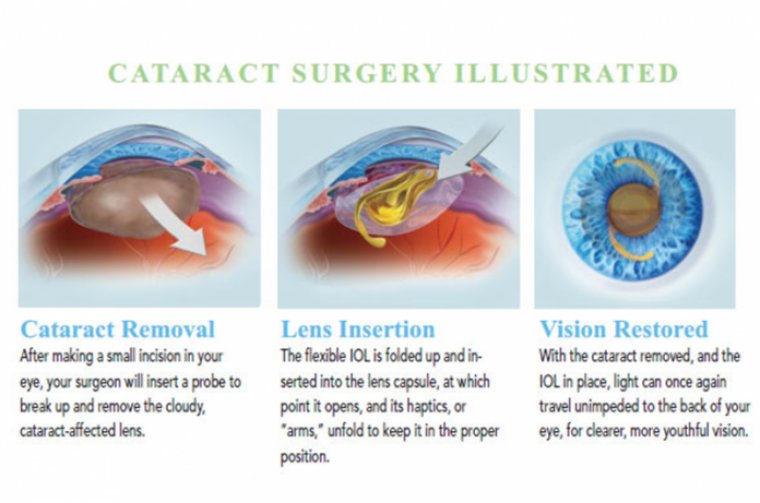
Aetna’s decision to require prior authorization of all cataract surgery procedures went into effect July 1, 2021. This policy created “burdensome amounts of work for ophthalmic practices, resulting in tens of thousands of delayed cataract surgeries and even denials for some patients when the procedure was medically necessary,” according to the ASCRS announcement.
ASCRS and AAO engaged in a joint public relations campaign with Schmidt Public Affairs that ultimately resulted in 200 targeted media placements inside the beltway and in media markets nationwide that “helped educate the public about the negative impact this policy had on physicians, as well as the dangers of delayed and denied care for Aetna beneficiaries,” according to ASCRS.
In addition, ASCRS and AAO held several meetings with Aetna leadership, questioning the policy’s necessity, detailing the difficulties with rollout and issues with compliance.