Pre-existing Astigmatism & Cataract Surgery
Irregular astigmatism occurs when the angle between the axis of maximum curvature and minimum curvature is not a right angle or when the curvature of a refractive surface is not axially symmetric, and often cannot be corrected with spectacles.
There have been reports of effective outcomes after toric IOL implantation in patients with corneal conditions that are associated with irregular astigmatism, including mild or moderate keratoconus, postkeratoplasty, pellucid marginal degeneration, and postpterygium.
It is possible that certain types of irregular astigmatism could be corrected by toric IOL implantation.
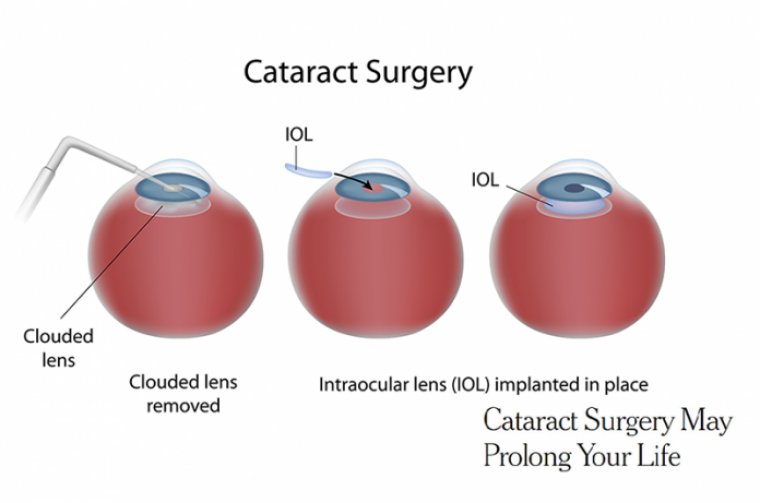
Cataract is a common cause of visual impairment and one of the main causes of blindness worldwide. Preexisting corneal astigmatism of >1.0 D has been reported to be present in 23%–47% of eyes with cataract.
Corneal astigmatism is typically regular but may be irregular. Toric intraocular lenses (IOLs) are widely used to treat corneal astigmatism and cataract and are an effective and safe treatment for patients with both conditions.
Toric IOL implantation has been reported to have a corrective effect on patients with cataract and regular corneal astigmatism. However, some patients with cataract have irregular astigmatism.
Uncorrected astigmatism can not only lead to decreased vision but also a decline in quality of vision and quality of life. Therefore, it is important to be able to minimize residual astigmatism postoperatively.
Eyes that have pre-existing irregular astigmatism and cataract present a unique difficulty and, at the same time, opportunity to improve vision beyond what the patient has ever achieved with spectacle correction.
These patients who have corneal pathology may complain of glare, halos, loss of best-corrected visual acuity, and/or loss of contrast sensitivity that is additive to the disability created by the cataract.
As a result, they often cannot be satisfactorily rehabilitated with glasses or soft contact lenses post-cataract surgery. Essentially, eyes that have irregular astigmatism will almost, by definition, have the same visual problems after cataract surgery as they did prior to the development of their cataract.
A toric IOL may improve quantity of vision in preexisting irregular astigmatism, but it does not improve quality of vision because of the continued higher-order aberrations. A significant advance in refractive corneal surgery has been the ability to treat irregular corneas.
In fact, there are now several technologies refractive surgeons are able to utilize to significantly improve the regularity of irregular corneas in patients contemplating cataract surgery and, in doing so, improve patients’ vision beyond not only their cataract formation but what they had prior to their development of corneal disease.
Here, we focus on the benefits of excimer laser technology and excimer laser PRK with riboflavin corneal crosslinking (CXL) in patients who have pre-existing irregular astigmatism.
Excimer Laser Benefits
With the use of the excimer laser as both a therapeutic and a refractive treatment, many times, these patients will no longer need to wear gas permeable lenses, but can wear soft contact lenses or glasses.
On occasion, these patients can even go spectacle-free. To review, the two types of excimer laser procedures are wavefront aberrometry-guided and topography-guided.
Here are the benefits of each:
Wavefront aberrometry-guided. The success with wavefront aberrometry to regularize the cornea is dependent on the ability of the aberrometer to capture an image suitable for treatment.
For patients who have mild corneal irregularities, performing a wavefront aberrometry excimer laser ablation treats the entire visual system, including the anterior and posterior cornea.
As a result, this can be utilized for forme fruste or mild cases of keratoconus, as well as for corneal scarring and other mild corneal irregularities.
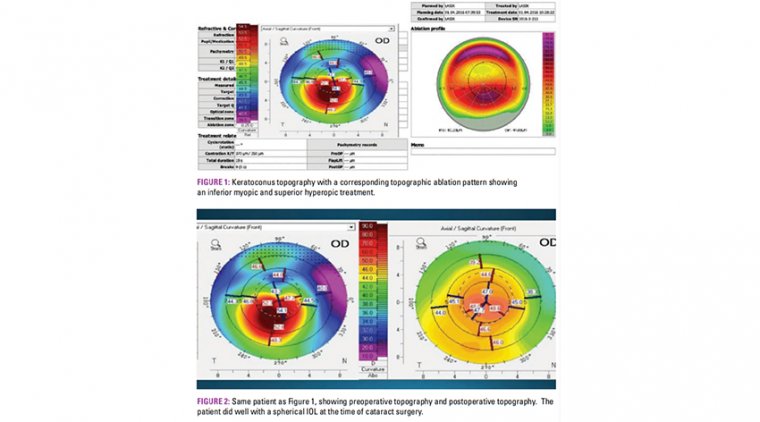
Topography-Guided (TG). For more irregular corneas, topographic excimer laser ablations have allowed refractive surgeons to treat irregular corneas that range from mild to moderate keratoconus.
As with wavefront aberrometry ablations, the key aspect is whether a treatable image can be captured for topographic ablation. TG laser ablations combine myopic and hyperopic ablations to create a more regular corneal surface.
They can flatten the steep areas of the cornea and steepen the flat areas of the cornea, so that we can improve patients by up to 10 D of corneal irregularity on a fairly routine basis.
We have found that we can often capture images in patients who have corneas as steep as 60 D in the device we use. The ability to capture an image is directly related to the steepness and regularity of the cornea.
Corneas that have keratometries of less than 50 D have almost a 100% success rate, while the capture rate decreases to less than 50% for corneas that have a keratometry of 60 D.
Excimer Laser With CXL
The TG and wavefront aberrometry PRK is preferred on irregular astigmatism patients because these patients almost always have thinner corneas, as well as irregular topographies.
In general, the more irregular the cornea, the deeper the ablation required to regularize the cornea. Although the likelihood of ectasia after PRK is much less than after LASIK in these patients, there is a concern regarding patients who have thin, irregular corneas; specifically keratoconus and pellucid marginal degeneration.
The ectasia after PRK can present much later and can lead to late diagnosis. For this reason, we perform riboflavin CXL to stabilize the cornea on all these at-risk patients who are considering excimer laser ablation followed by cataract surgery.
The advantage of simultaneous CXL and PRK is one less procedure day, shortening the rehabilitation by 3 months. The PRK is performed first, and the CXL is performed on the deeper tissue that remains.
The advantage of sequential treatment is that CXL often regularizes and flattens the cornea, creating a better ablation pattern, but the major advantage we have seen is that it prevents the delayed healing problems and occasional scarring that can occur with the insult to the cornea of same-day CXL and excimer laser ablation.
My colleagues and I favor a sequential approach and recently published the largest U.S. case series showing the safety and efficacy of TG-PRK in keratoconus patients after CXL.
Specifically, we found that leaving the epithelium on is more comfortable, reduces postoperative complications, and increases the pachymetry of the treated cornea for these thinner corneas. Briefly, a modified epithelium-on technique is performed following ocular surface anesthetization via drops.
A cotton-tipped applicator is then gently rolled over the corneal surface to create punctate epithelial erosions to improve riboflavin penetration. Riboflavin 0.5% solution without dextran is applied to the operative eye every 2 minutes for 1 hour and observed for stromal riboflavin absorption and flare in the anterior chamber.
Additional riboflavin is applied, and the cornea is reevaluated prior to proceeding to UV light application, if inadequate absorption is noted. CXL is then performed for 30 minutes.
Next, a bandage contact lens is placed, and the patient is given a topical flouroquinolone q.i.d. until epithelial closure, corticosteroid drops q.i.d. for 1 week and qd for 1 week, as well as NSAID drops b.i.d. for 3 days.
All patients are followed closely to ensure proper healing. Once stabilized (i.e., no significant change in refraction or topography for at least 3 months post-CXL), TG-PRK is performed.
The refractive goal of performing the procedure on patients planning on sequential cataract surgery after excimer laser ablation is to treat corneal topographic irregularities and astigmatism, but not the sphere, to minimize the tissue removed with the ablation.
The greatest concern for patients is that this is a sequential procedure that requires CXL followed at least 3 months later by excimer laser ablation and then another 3 months or more before cataract surgery can take place.
Therefore, the full rehabilitation requires at least 6 months. For patients undergoing excimer laser ablation for irregular corneas who are not planning on cataract surgery, we take into account the sphere to reduce myopia, but when subsequent cataract surgery is planned, the IOL can effectively correct spherical refractive error and reduce the need for a deeper corneal ablation.
In these patients, we reduce the cylinder as much as possible and regularize the topography, so that a toric IOL can be used to correct residual astigmatism.
The limits of the sequential procedure include maximum astigmatic correction of 3.00 D for topographic ablations and 5.00 D for wavefront treatments in the U.S., based on current FDA restriction.
Topographic irregularities are addressed if excimer laser treatment of refractive error leaves a calculated residual stromal bed of more than 300 μm.
A very effective way to reduce the depth of the ablation is to reduce the optical zone size, which is not a problem in these patients, due to the smaller pupil size following cataract surgery.
For phakic patients, my normal optical zone ablation is 6.5 mm for topographic treatments and 6.0 mm for wavefront treatments. For patients for whom cataract surgery is contemplated, we reduce the optical zones by 0.5 mm to 6.0 mm for wavefront treatments and 5.5 mm for wavefront treatments.
In patients who are not candidates for TG or wavefront aberrometry PRK because a treatable image cannot be captured, the cone can be flattened using PTK with the excimer laser.
PTK flattens the cone and uses the epithelium to prevent ablation in the flatter areas, while the cones that have thinner epithelia over their surface ablate more rapidly.
Very commonly, this can flatten the cone by up to 5 D. Many times, we have followed this procedure with a topographic ablation several months later.
Improving Vision
The combination of CXL, excimer laser ablation and cataract surgery combines multiple technologies that allow the corneal/ cataract surgeon to improve the vision in patients who have preexisting irregular corneas and cataracts.
We have utilized this technique and demonstrated significant improvement in vision. For IOL power calculation, we utilize a conventional IOL formula.
Although these patients may not lose their spectacles, the goal is to dramatically improve their best-corrected vision by reducing their corneal irregularities and astigmatism and, ultimately, improve their quality of life.