Risk Factors for Developing Endophthalmitis After Cataract Surgery
The prevalence of postprocedural endophthalmitis has increased in recent years, due in part to a wider range of indications for ophthalmic procedures, better access to treatments and therefore an increase in the overall number of surgical interventions being performed.
Although postprocedural endophthalmitis is a rare event, endophthalmitis is always a devastating complication for both the patient and surgeon. Prompt diagnosis and effective treatment are necessary to increase the likelihood of a good visual outcome.
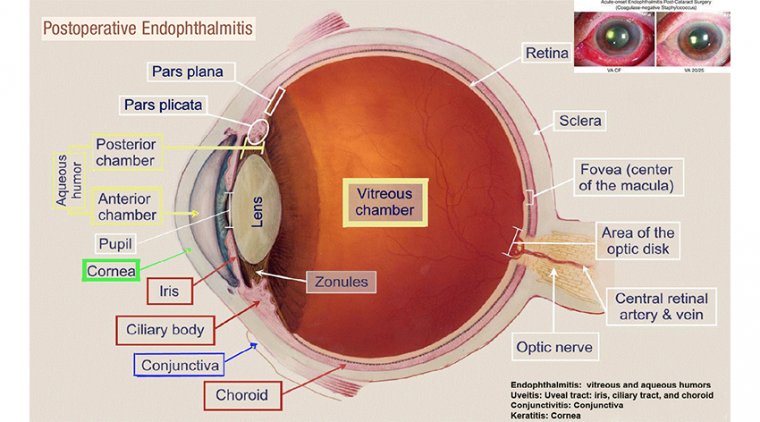
Endophthalmitis is a devastating complication that can occur after any ocular surgery. It has been associated with both intraocular and extraocular procedures.
Despite low rates of endophthalmitis associated with each ophthalmic procedure, it is a severe and sight-threatening complication with a rising prevalence.
This increase in prevalence is likely related to the greater number of procedures performed, an aging patient population, antibiotic resistance and pathogen virulence.
In addition, the past decade has seen major shifts in clinical interventions, including much expanded use of intravitreal injections and the emergence of novel corneal surgeries. The overall postprocedural endophthalmitis rate ranges from 0.05 to 0.3%.
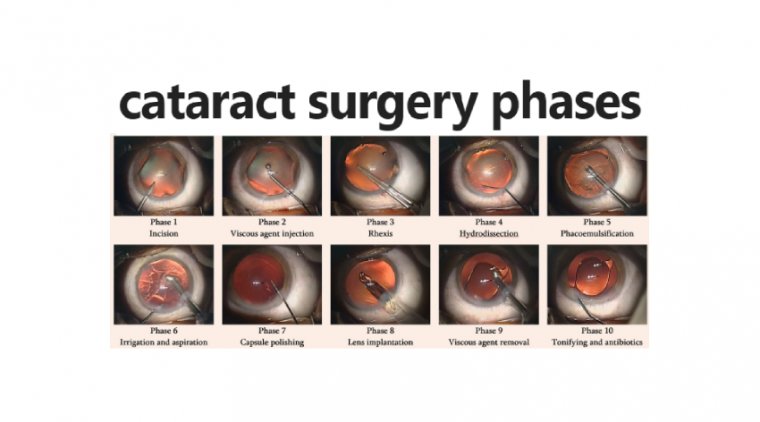
Cataract surgery remains the most commonly performed ophthalmic surgery and the leading cause of postoperative endophthalmitis.
However, endophthalmitis has also been reported after glaucoma surgery, pars plana vitrectomy, intravitreal injection, corneal transplant and keratoprostheses, and virtually all other ophthalmic procedures.
Cataract surgery is the most common cause of endophthalmitis, accounting for 70% of cases of postsurgical endophthalmitis.
The reported incidence of acute endophthalmitis after cataract surgery ranges from 0.001 to 0.3%. The number of endophthalmitis cases is rising around the world, secondary to overall increased number of procedures performed.
Acute-onset endophthalmitis by definition occurs within 6 weeks of surgery; however, most cases present within 1–2 weeks. Patients experience decreased vision and eye pain.
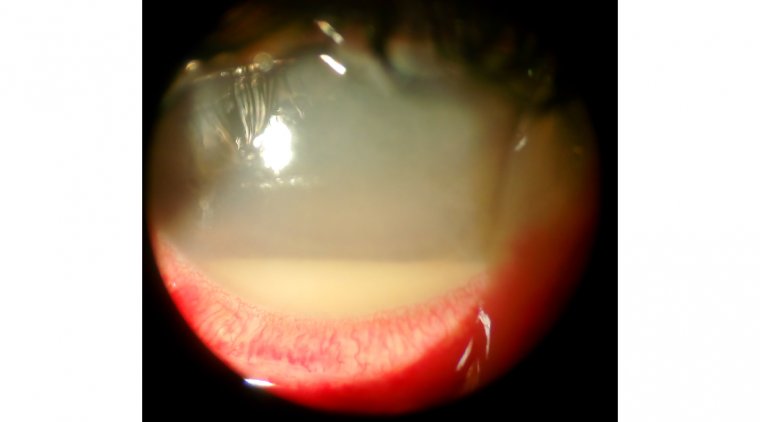
Ocular signs include conjunctival injection and intraocular inflammation ranging from mild inflammation to severe panophthalmitis with hypopyon and no view to the posterior pole.
Wound abnormalities, including leakage and vitreous incarceration, suggest possibility of infectious contamination.
B-scan ultrasonography is a useful tool to help identify vitreous inflammation caused by infection and associated complications of endophthalmitis such as development of choroidals and retinal detachment.
It is important to differentiate postcataract endophthalmitis from other pathologies such as toxic anterior segment syndrome.
Toxic anterior segment syndrome can mimic endophthalmitis, however, it usually occurs within 24 h of surgery, is associated with little or no ocular pain, involves limbal-to-limbal corneal edema and no inflammatory involvement of the vitreous.
The risk factors for development of endophthalmitis after cataract surgery have been identified as complex cataract procedures, the performance of simultaneous vitreous procedures, a history of diabetic macular edema or proliferative diabetic retinopathy, male sex, and certain cataract types.
A large retrospective analysis using the IRIS (Intelligence Research in Sight) Registry showed that these factors are associated with significantly higher rates of endophthalmitis, according to Michael H. Goldstein, MD, president and chief medical officer of Ocular Therapeutix Inc.
Endophthalmitis is rare after cataract surgery, but it does occur and is vision threatening, with incidence rates ranging from 0.5 to 3.0 cases per 1000 cataract surgeries.
Goldstein pointed out that the incidence rate between 2013 and 2017 was 0.42 cases per 1000 surgeries based on IRIS Registry data.
The investigators also wanted to determine if use of the ReSure Sealant impacted the incidence rate of endophthalmitis one way or the other.
This hydrogel sealant creates an in situ temporary soft-surface barrier to prevent wound leaks from clear corneal incisions up to 3.5 mm in size following cataract surgery.
Goldstein and colleagues conducted a retrospective analysis of IRIS Registry data to compare the incidence of endophthalmitis within 30 days of any cataract procedures performed with and without the ReSure Sealant and to identify the incidence of endophthalmitis within 30 days after any cataract surgery performed in the US.
Study Design/Results
This study was a post hoc analysis of patients who underwent cataract surgery from January 1, 2016, to December 1, 2019. All patients were 22 years or older and underwent phacoemulsification with intraocular lens implantation and had completed 1 or more visits within 30 days postoperatively.
Practices must have provided data for 30 days or more after surgery. All data were collected from the IRIS Registry (P < .001 was considered significant).
“This study was one of the largest recent data analyses performed to determine the incidence of acute postoperative endophthalmitis after cataract surgery,” Goldstein said.
Data from more than 6,700,000 eyes (4.1 million patients; 58.9% women; mean age, 70.91 years) were included in the study. More than 3.5 million eyes underwent surgery at practices where ReSure Sealant was available.
Almost three-fourths of patients were Caucasian. Approximately 93% of cases were routine, and the remaining ones were considered complex.
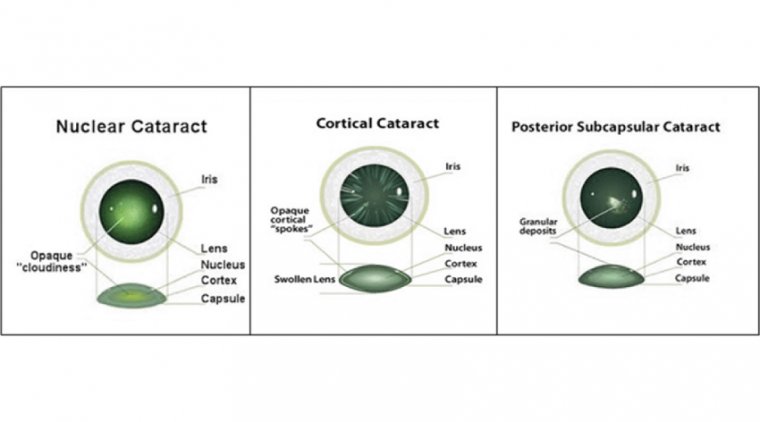
Two-thirds of the cataracts were the nuclear sclerotic type, and the rest in descending order were cortical, posterior subcapsular, congenital, and traumatic.
Glaucoma procedures were performed concurrently in approximately 3.5% of cases and vitreous procedures in approximately 0.5% of cases.
Slightly more than 20% of patients had a history of diabetes. Goldstein reported that the overall incidence of endophthalmitis was 0.633 case per 1000 surgeries (95% CI, 0.614-0.652).
When the data were stratified by the type of cataract, the incidence of endophthalmitis was significantly higher after complex procedure compared to routine procedures: 1.148 vs 0.592 case per 1000 surgeries, a difference that reached significance (P < .0001).
When the data were analyzed based on the use or no use of ReSure Sealant, no significant difference was found in the incidence of endophthalmitis: 0.609 vs 0.660, respectively, which did not reach significance (P < .01).
The specific clinical risk factors that the data analysis identified in association with higher incidence rates of endophthalmitis were complex cataract procedures (odds ratio [OR], 1.67; P < .0001); concurrent vitreous procedures (OR, 4.32; P < .0001); traumatic (OR, 4.84; P < .0001), nuclear sclerotic (OR, 1.18; P < .0001), and posterior subcapsular (OR, 1.21; P < .0001) cataracts; and a history of proliferative diabetic retinopathy (OR, 1.53; P < .0001).
In addition, male sex (OR, 1.19; P < .0001) was also identified as a significant risk factor, as was multiethnicity (OR, 2.60; P < .0001).
“These results provide risk factors for endophthalmitis after cataract surgery from 2016 to 2019 and can help identify patients at high risk of developing endophthalmitis after cataract surgery,” Goldstein concluded.