Phacoemulsification With or Without Ultrasound Ciliary Plasty in Coexisting Cataract and Open-Angle Glaucoma
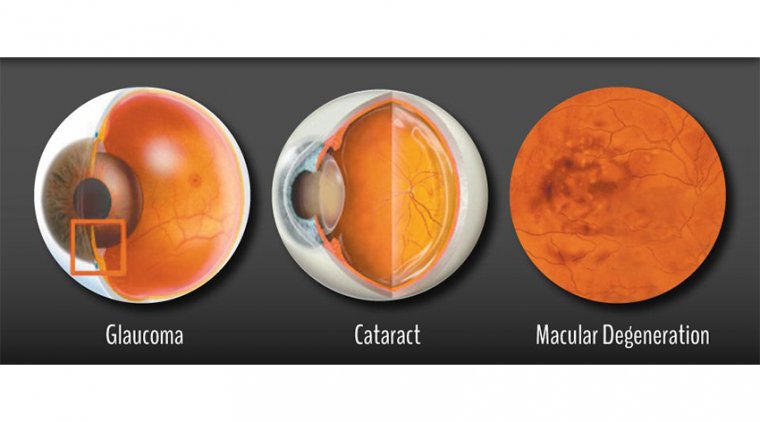
Cataract and glaucoma are leading causes of blindness all over the world (51 and 8%, respectively), that frequently coexist in the same eye.
Cataract surgery has been found to decrease the intraocular pressure (IOP) in both normal and glaucomatous eyes, by an average of 1.5–4 mmHg. However, this reduction is influenced by many factors including preoperative IOP, angle configuration and type of glaucoma.
IOP reduction is more with higher preoperative IOP and in eyes with closed angles more than those with open angles. In eyes with moderate to advanced open angle glaucoma, relying on phacoemulsification alone to reduce IOP may not be sufficient.
In addition, the effect of IOP reduction after phacoemulsification alone is known to regress over time. Moreover, IOP spikes after phacoemulsification is one of the feared complications in moderate and advanced stages of glaucoma.
Many glaucoma surgeons recommend a combined procedure for patients with significant cataract and glaucoma requiring urgent drainage surgery.
Phaco-trabeculectomy (Phaco-trab) has been traditionally shown to be effective, but might be associated with significant complications, the commonest of which are hypotony, hyphema, and shallow anterior chamber.
Recently, various microinvasive glaucoma surgeries (MIGS) have been described, to be combined with cataract surgery, aiming for an additional reduction of IOP and hence, decreasing the burden of anti-glaucoma medication (AGM).
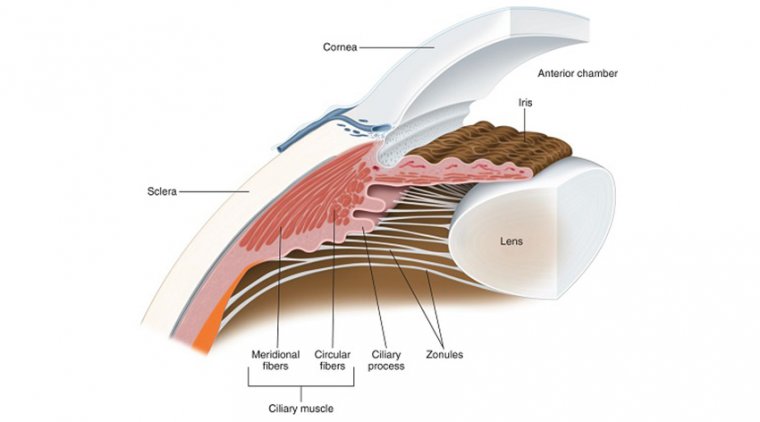
Ultrasound ciliary plasty (UCP) is a recent non-incisional technique recommended for primary and refractory glaucoma. It involves inducing selective coagulation of the ciliary epithelium using the high intensity focused ultrasound technology (HIFU).
It has the advantages of being easy, one-step, highly reproducible, and more precise treatment.
This study was carried out to evaluate the safety and efficacy of combined phacoemulsification and Ultrasound ciliary plasty (Phaco-UCP) as a first-line surgical treatment for coexisting cataract and open angle glaucoma, compared to phacoemulsification alone (Phaco-alone).
Further exploring the effect of concurrent glaucoma surgery and cataract surgery in patients with glaucoma, Magda A. Torky, MD, and colleagues led a clinical trial to examine the safety and efficacy of ultrasound ciliary plasty (UCP) combined with phacoemulsification for managing coexisting cataract and open-angle glaucoma (OAG).
Published in BMC Ophthalmology, the study found that, compared to phacoemulsification alone (Phaco-alone), combined phacoemulsification and UCP (Phaco-UCP) appears safe and more successful in reducing intraocular pressure (IOP) and glaucoma medication use.
According to the authors, the results suggest that the combination of phacoemulsification and UCP surgeries is an effective primary surgical treatment option for treating primary and refractory glaucoma patients.
The study was conducted on 61 eyes of 61 patients with visually significant cataract and OAG. Subjects were randomized to either the Phaco-UCP study group (n = 31) or the Phaco-alone control group (n = 30).
Primary endpoints assessed were IOP reduction and/or reduction in the number of glaucoma medications needed. Secondary endpoints included vision improvement and post-surgery complications.
Treatment outcomes were analyzed up to 18 months postoperatively, with success defined as an IOP reduction of ≥ 20% from the baseline to a range of 6 to 21 mmHg with no additional glaucoma medication or surgery.
Serious complications, the need for more surgical treatments, or an IOP reduction of < 20%, despite medication use, all constituted a treatment failure.
The Phaco-UCP group had a significantly higher success rate at all follow-up points, reaching 67.7% at final visit, versus just 16.7% in the Phaco-alone group (p < 0.001).
At 18 months, the Phaco-UCP group recorded a median IOP reduction of 7 mmHg, compared to 2 mmHg in the Phaco-alone group (p < 0.001).
The median number of glaucoma medications used also significantly decreased from preoperative baselines of three in each group, to one and two at 18 months (p = 0.3 and p < 0.001, respectively). No serious complications were encountered in either group during the study.
This first report on combined Phaco-UCP finds the technique to be “simple, safe, and effective” for treating patients with coexisting cataract and OAG, introducing greater IOP and medication usage reduction over stand-alone phacoemulsification, without sacrificing favorable outcomes from phacoemulsification alone, the authors concluded.