Cataract Surgery for Children & The Role of Femtosecond Laser
Congenital cataracts and childhood cataracts are not very common. However, in the event that a child or infant has cataracts, it is not easy to predict how much their vision will be improved after the treatment.
In most cases, children tend to have a reduction in vision even after the treatment.
Cataract surgery is the most common treatment for children with cataracts. When it is performed on children and babies, the procedure will be performed under general anesthesia.
The procedure will take a longer time than it does for an adult and may take up to one or two hours. If the cataracts are present at birth, doctors will usually recommend that surgery be done as early as a few weeks after birth.
The procedure starts with the doctor applying eye drops to dilate the pupil. Then, a small cut is made on the cornea to allow for the cloudy lens to be removed. The next step is to install an intraocular lens (IOL) to replace the removed lens.
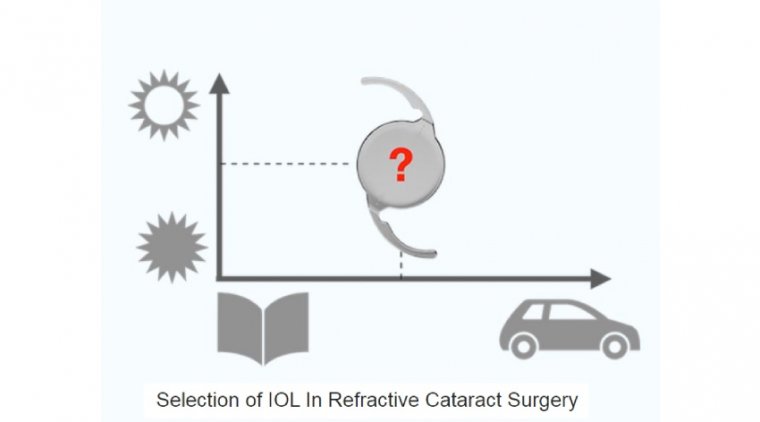
The IOL will restore the eye’s focusing ability that is lost with the removal of the lens. However, it is more common for young children and babies to not get an IOL implant right away. The best option for them is to choose removable contact lenses or eyeglasses.
These can be chosen and fitted about a week or two after the surgery. After the procedure is complete, the incision on the cornea will be closed.
For children or infants with cataracts, the risk of further complications after cataract surgery is a bigger possibility. With the fitting of an IOL, treating complications that may occur later on can get difficult.
In fact, there have been reports of IOLs being the cause of the complications. Therefore, removable contact lenses or specially designed eyeglasses are the better option with better long-term results.
It is quite normal for a child or infant to stay overnight after a cataract surgery.
This way, their recovery can be closely monitored. In the event of bilateral cataracts (cataracts in both eyes), the surgeon will work separately on each eye to minimize the risk of complications. In this case, the operations will be conducted about a week apart.
After the operation, regular check-ups are a must to monitor the progress. A child’s vision will develop as they grow, and the strength of the glasses or contact lenses will be adjusted accordingly.
Performing cataract surgery on very young children comes with several challenges, partly due to the anatomical peculiarities of an eye that may be just a few weeks old but mainly because the initial operation is usually just the first of numerous interventions that may be necessary over the next few years to give the patient a chance of developing normal, healthy vision.
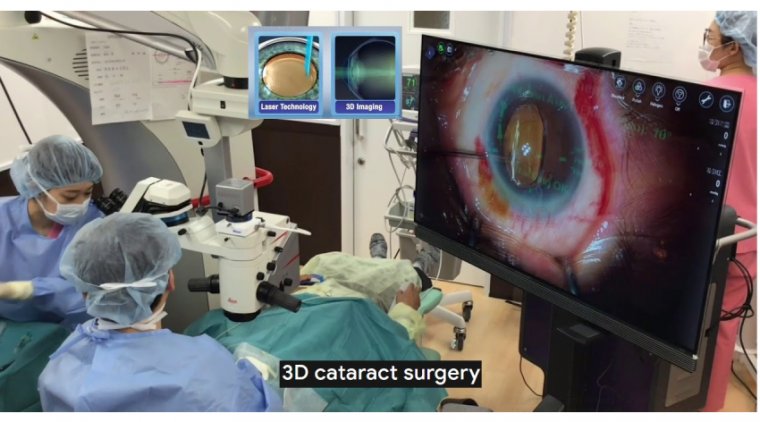
The femtosecond laser can play a crucial role in achieving this goal. We were one of the first centers to employ the femtosecond laser in pediatric cataract cases, which is, as with many interventions in our youngest patients, an off-label procedure or contraindication for most laser platforms (the Ziemer laser system is the exception because it has a CE mark for laser cataract surgery in pediatric cases).
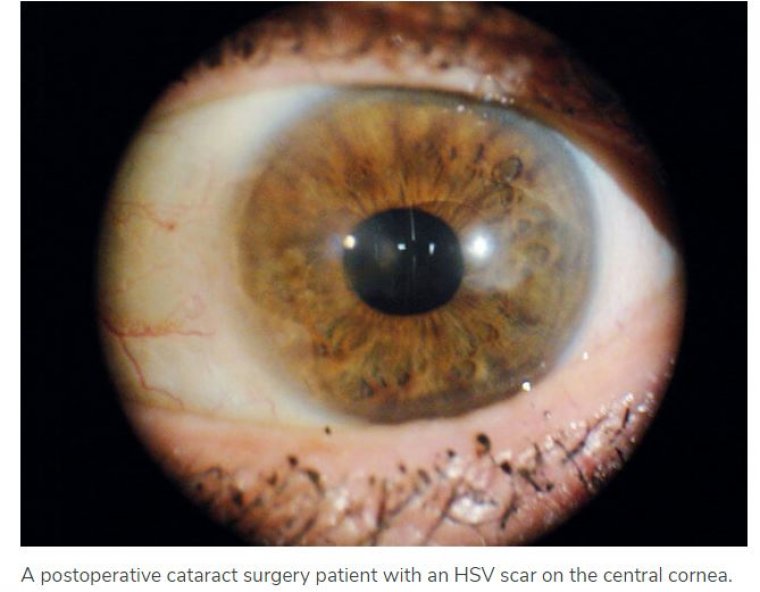
There are some things in pediatric cataract surgery that the surgeon must be aware of before planning the intervention. There will be soft eye tissues with a low scleral rigidity, and the operation—and often the pre- and postoperative examinations—will have to be performed under general anesthesia.
There likely will be a high degree of difficulty in calculating the appropriate IOL power (if IOL implantation is intended). Automated keratometry will be necessary, and another consideration is that posterior capsule opacification (PCO) may develop in a relatively short time after surgery.
This complication is almost guaranteed to occur if the posterior capsule is left intact. Finally, the surgeon must be able to perform a vitrectomy.
Risks versus benefits
Choosing the best possible time to operate on a newborn or a very young child always means weighing the risks and benefits. After early surgery, massive axial elongation and a substantial myopic shift can be expected.
Operating at a very young age increases the likelihood of the major postoperative complication of glaucoma. This and other postoperative complications occur at a much higher incidence when surgery takes place when a patient is younger than 4 weeks.
A general recommendation might be—with necessary caution—that unilateral congenital cataract should be operated upon 4 to 6 weeks after birth and bilateral cataract done at 6 to 10 weeks after birth.
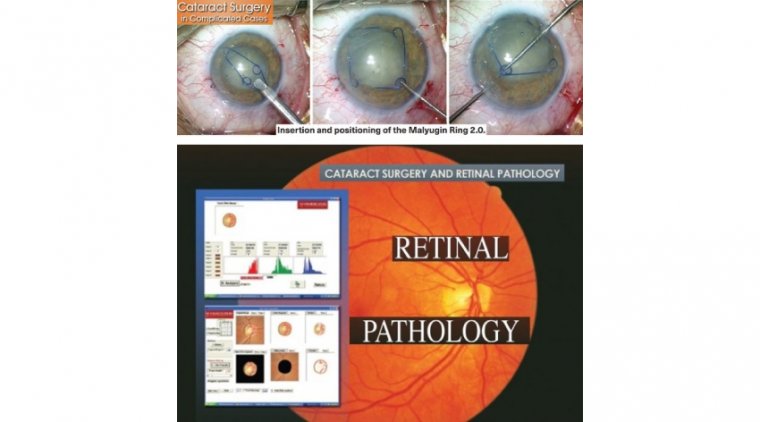
Unlike in cataract surgery in adults, we do not employ the laser for lens fragmentation (this is done by aspiration) but primarily to achieve a perfect capsulotomy— anterior as well as posterior—which is essential, and not only when primary IOL implantation is intended.
With anterior capsulotomy as a crucial step in the operation and for postoperative visual recovery, we were satisfied with even our first pediatric laser cataract surgery cases when we found an optimal circularity of femtosecond-laser–created anterior and posterior capsulotomies.
As expected, the size of the capsulotomy initially did not turn out as planned because of the elasticity. There was considerable widening of the capsule opening immediately after laser treatment. With experience, we found that, particularly in very young children, the capsulotomy diameter tends to turn out larger than planned.
In a clinical series involving 22 eyes of 18 patients, we were able to develop the Bochum formula, which corrects for this aberration. A desired capsulotomy diameter can be achieved using the following formula: programmed diameter = aimed diameter (1.34 + (-0.009 age))
Preventing opacification
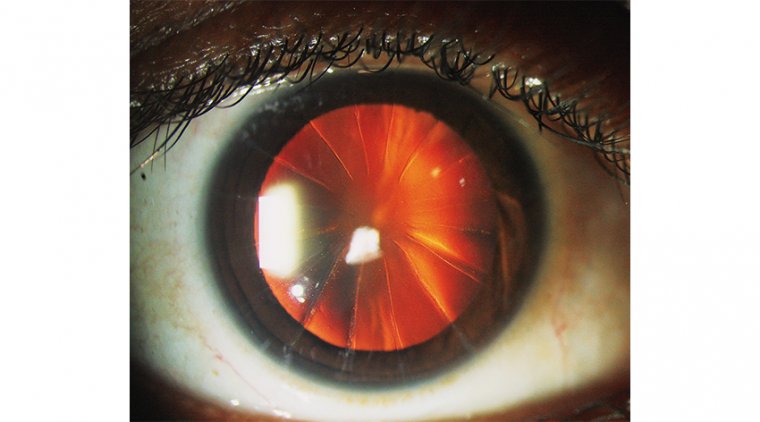
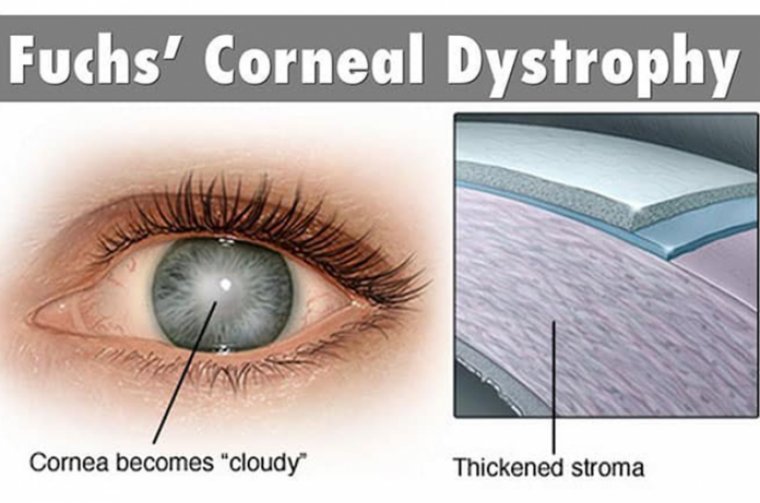
A true bane of pediatric cataract surgery is the high incidence of PCO. A special surgical technique—more for the experienced surgeon than for the newcomer—has the potential to considerably reduce the chance of this complication developing.
First described by Marie-José Tassignon, MD, in 2002, during bag-in-the-lens (BIL) technique the anterior and posterior capsules are placed in a special IOL’s flange after creating both an anterior and a posterior capsulotomy with the femtosecond laser.
The laser is particularly crucial for creating a perfectly centered posterior capsulotomy. The IOL used is a foldable hydrophilic 1-piece IOL that is completely inserted and unfolded in the anterior chamber.
Its posterior haptics are placed behind the posterior capsule and the anterior haptics are positioned in front of the anterior capsule. This prevents the proliferation and migration of lens epithelium cells over the long term and thus prevents PCO.
The femtosecond laser may make this manually challenging technique an option for surgeons who have not previously implanted BIL lenses. The femtosecond laser can safely perform the posterior capsulotomy and keep the anterior hyaloid membrane intact.
Special needs
For patients with special needs, there are additional preoperative considerations. For instance, patients with Down syndrome have a higher incidence of childhood cataract than the general population.
But as Saifee et al7 stated based on their experience, cataract extraction in pediatric patients with Down syndrome does not appear to have a higher rate of surgical complications than does cataract surgery in the general pediatric population.
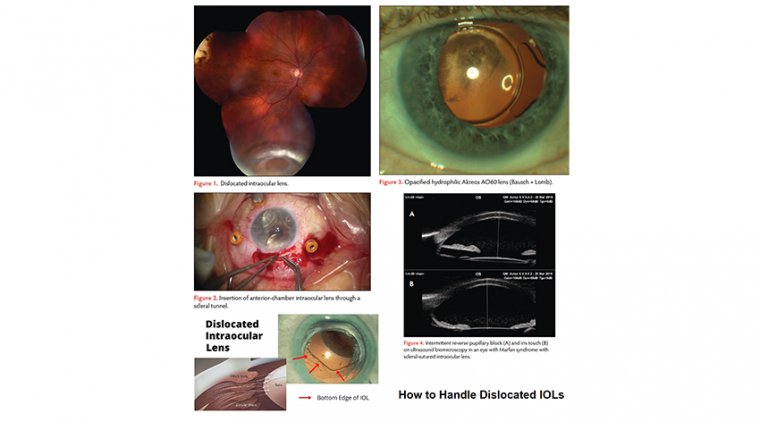
There is no reason to assume that laser cataract surgery in these patients might be less effective or less safe than in children without this condition. Patients with Marfan syndrome may need surgery of the lens even when they do not have a cataract.
Their vision is often compromised by a subluxation of the lens that may render the visual axis aphakic by irregular astigmatism from the lens periphery and also occasionally from lens opacity. Lens removal with capsule fixation and IOL implantation is a valuable strategy to address these problems.
However, as in the younger patients with congenital cataract, challenges with manual capsulorhexis result from the high elasticity of the capsule (which has a tendency toward posterior tears), damage to the zonules from stress during manipulation, and the fact that the desired position for capsulorhexis is off center, all too often resulting in increased intraoperative complications for these patients who undergo surgery at a relatively young age.
Early experience
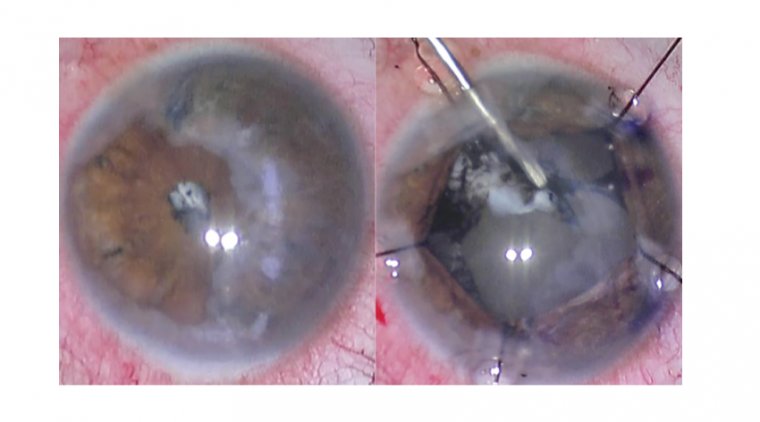
In one of the first cases treated with a femtosecond laser, we operated on a 10-year-old boy with ectopia lentis in both eyes, employing the femtosecond laser in the right eye under general anesthesia.
After the ocular surfaces were identified with the integrated algorithms, the capsulotomy was automatically placed by the software at the center of the scanned capsule, which was at the superior, temporal periphery of the pupil.
The selected capsulotomy diameter was 4.1 mm (incision depth: 1000 μm). No lens fragmentation was performed. The total suction time was 2 minutes and 45 seconds.
A microforceps was used to remove the capsular disc, and no radial tears were noted. The soft lens was aspirated with standard bimanual irrigation/aspiration devices.
No complications were observed within 10 weeks of follow-up.8 Given the fact that pediatric laser cataract surgery for most laser platforms is off label, there are still shortcomings that hopefully will be overcome in the near future.
There is no software adapted for posterior capsulotomy, which makes it necessary to position the treatment zones manually. Only 2 laser platforms (Johnson + Johnson Vision and Ziemer) come with an interface for a smaller eye.
There is no special formula for choosing the appropriate IOL for our youngest patients: all of them have been created for adults. Experience has shown the Barrett formula to be more reliable than other formulas.
It is worth noting that the ideal target refraction in very young infants seems to be a slight myopia as they primarily focus on near objects such as their toys or their mother’s face.9
Continuous follow-up
The operation is the first step to visual recovery for a child with cataract, to be followed by longterm care provided by the ophthalmologist.
The parents (or caregivers) must be educated about the need for continuous follow-up so that complications such as inflammation, glaucoma, and PCO can be detected and treated as soon as they arise, refractive errors can be corrected, and amblyopia therapy can be pursued.
For this first step, we should use all our expertise and the best technology available. In my view, this is—more often than not—the femtosecond laser.