Fuchs’ Dystrophy & Cataracts
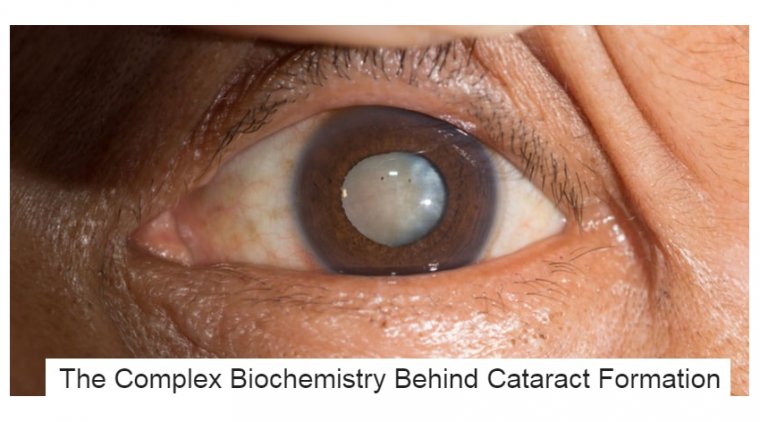
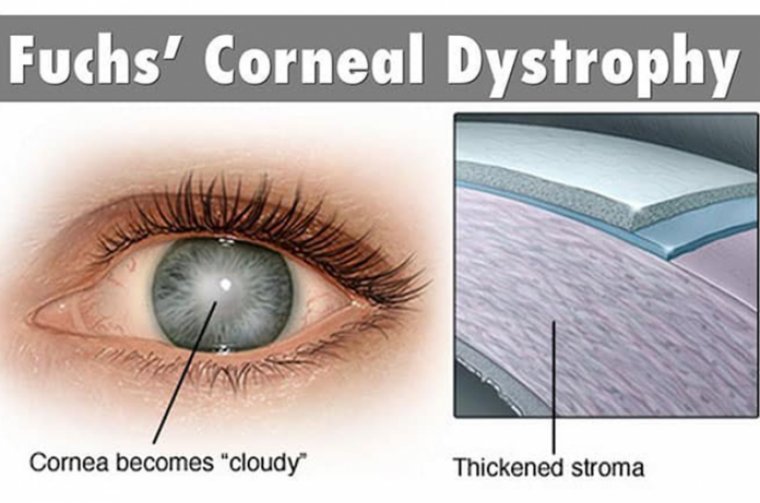
Fuchs’ dystrophy is a disease of the cornea. It is when cells in the corneal layer called the endothelium gradually die off.
These cells normally pump fluid from the cornea to keep it clear. When they die, fluid builds up and the cornea gets swollen and puffy. Vision becomes cloudy or hazy.
Fuchs’ dystrophy has two stages. In the early stage (stage 1), vision is usually hazy in the morning. With the later stage 2, vision remains blurry all day.
People in their 30s and 40s may have Fuchs’ dystrophy but not know it. Vision problems might not appear until age 50 or later. Women are more likely than men to have Fuchs’ dystrophy. Family history of Fuchs’ dystrophy also increases your risk of developing it.
What Are Fuchs’ Symptoms?
In the early stage (stage 1) of Fuchs’ dystrophy, you may notice few, if any, symptoms. Your vision may be hazy or blurry when you first wake up but improve throughout the day. This is because
your eyes normally stay moist when they are closed during sleep. But when you are awake, the fluid dries normally.
In the later stage (stage 2), your blurry or hazy vision will not get better as the day goes on. Too much fluid builds up during sleep and not enough dries up during the day. Also, tiny blisters may form in the cornea. The blisters get bigger and eventually break open, causing eye pain. Here are other symptoms:
- Sandy or gritty feeling in your eyes
- Being extra sensitive to bright light
- Eye problems get worse in humid areas
- Very blurry or hazy vision from scarring at the center of the cornea
The landscape of keratoplasty has changed during the past decade. In 2012, endothelial keratoplasty (Descemet’s stripping endothelial keratoplasty [DSEK] and Descemet’s membrane endothelial keratoplasty [DMEK]) surpassed penetrating keratoplasty as the most frequently performed corneal transplant in the United States.
Just three years later, 27,208 endothelial keratoplasty (EK) and 19,160 penetrating keratoplasty (PK) were performed in the United States, according to the 2015 EBAA Statistical Report.
With this evolution in technique, corneal transplant for patients with Fuchs’ endothelial dystrophy may be offered earlier in the course of disease.
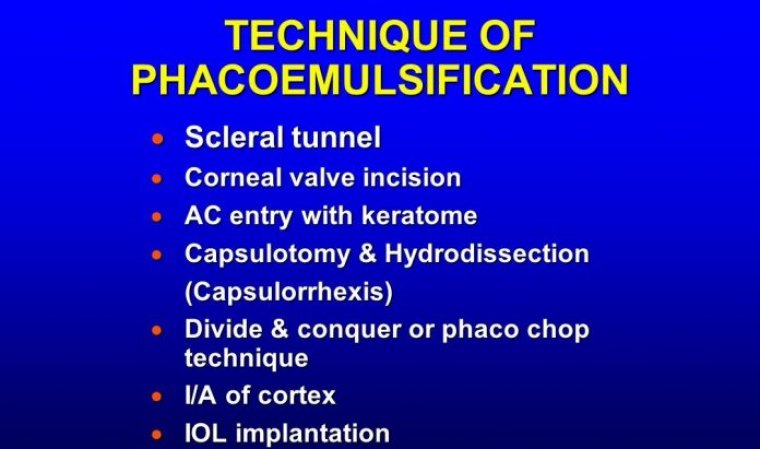
This evolution is much like cataract surgery being offered earlier after the movement from large incision extracapsular cataract extraction to small incision phacoemulsification.
Along with the smaller incision, EK provides more rapid wound healing, structural integrity of the globe, less rejection and faster visual recovery and quality compared to PK.
This has changed the conversation between patients and surgeons with respect to when to offer transplant, how to manage with incipient or concomitant cataract and setting realistic expectations.
These issues will continue to evolve with the increase of even more targeted treatment of endothelial disease with the thinner DMEK tissue. Here, we offer advice on when to perform cataract surgery and/or EK procedures for Fuchs’ dystrophy patients.
CATARACT SURGERY ALONE
For mild to moderate Fuchs’ dystrophy, we obtain baseline endothelial cell count and morphology as well as pachymetry.
In general, most patients in this category are able to undergo phacoemulsification alone with proper counseling that they may have a longer postoperative resolution of corneal edema and possible future need for EK.
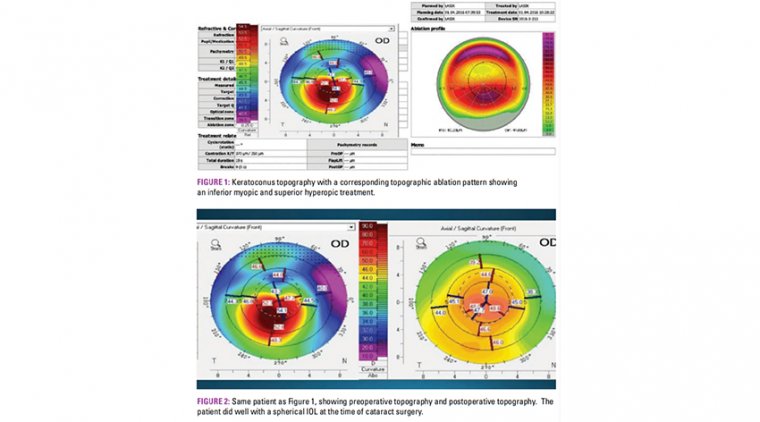
In preparation for the possibility of DSEK, consider a target postoperative refraction at about -0.75 D to -1.00 D since DSEK tends to produce a hyperopic shift in the +1.25-D range. DMEK (typically 15 μm thick and planar in configuration) also has a hyperopic shift, but less so than DSEK since there is no posterior stroma transplanted.
We stay away from multifocal and toric IOLs in these patients, since keratometry and biometry are less predictable in abnormal corneas in addition to the variable hyperopic shift produced by a future EK.
We recommend liberal use of dispersive viscoelastic to coat the endothelium and work in the middle of the eye, staying away from the endothelium. Additionally, we suggest judicious use of irrigation and phaco power.
EK ALONE
EK alone is an option in younger patients (under 50 years old) with a deep anterior chamber depth and clear lens in order to preserve accommodation. In addition, corneal edema may interfere with reliable keratometry, so consider EK first then phaco.
Severe corneal edema that prohibits visualization to remove the cataract is also an indication for EK first.
In patients older than 50 with a clear lens and deep anterior chamber, a more elaborate discussion of the pros and cons of EK alone vs. a combined procedure is warranted.
Just like the increased risk of cataract surgery shortly after retinal surgery, patients older than 50 who undergo EK have a higher risk of developing visually significant cataracts within three years, according to a 2014 Journal of Cataract and Refractive Surgery study by Burkhart et al.
In addition, if the anterior chamber depth is shallow, the chance of developing cataract following EK is higher.
COMBINED CATARACT AND EK PROCEDURES
Combined cataract and EK procedures are recommended in patients with any grade of cataract and a cell count/morphology/slit lamp exam that shows severe corneal disease predictive of persistent corneal edema postoperatively with phaco alone.
In addition, combined surgery is considered in situations such as patient’s desire to undergo one procedure or medically complex scenarios, such as patients having trouble lying flat or those with a significant anesthesia risk.
It is also important to consider the patient’s preference in undergoing a transplant and its attendant risk of rejection vs. delaying the need for donor tissue.
POSTOPERATIVE CONSIDERATIONS
Early postoperative considerations include graft dislocation, interface infection and endophthalmitis. Late postoperative considerations include graft rejection, interface infection and endophthalmitis (particularly fungal).
Report infections to the eye bank so the donor’s mate can be traced. In addition, if you obtain donor rim cultures at the time of transplant, keep in mind that a positive fungal culture has high concordance with clinical infection.
Currently, there is no consensus on best practices in response to a positive fungal culture. Options include close follow up or prophylactic anti-fungal treatment.
In general, we find that most patients can undergo gentle cataract surgery alone and counsel them that they may require EK down the road. Corneal surgery is being offered sooner — the wounds have become smaller and visual rehabilitation is more rapid.
Our understanding of visually significant corneal disease has evolved beyond Snellen acuity, with glare and morning blur being common corneal edema symptoms. These symptoms play a legitimate role in the decision to have corneal surgery.
Future studies include optimization of IOL calculations for EK patients, long-term follow up of DMEK, the emergence of Descemet’s stripping only without insertion of donor Descemet’s membrane and endothelium as well as cultured corneal endothelial cell therapy and Rho kinase inhibitors.