Relation Between Surgeon Age & Postoperative Outcomes
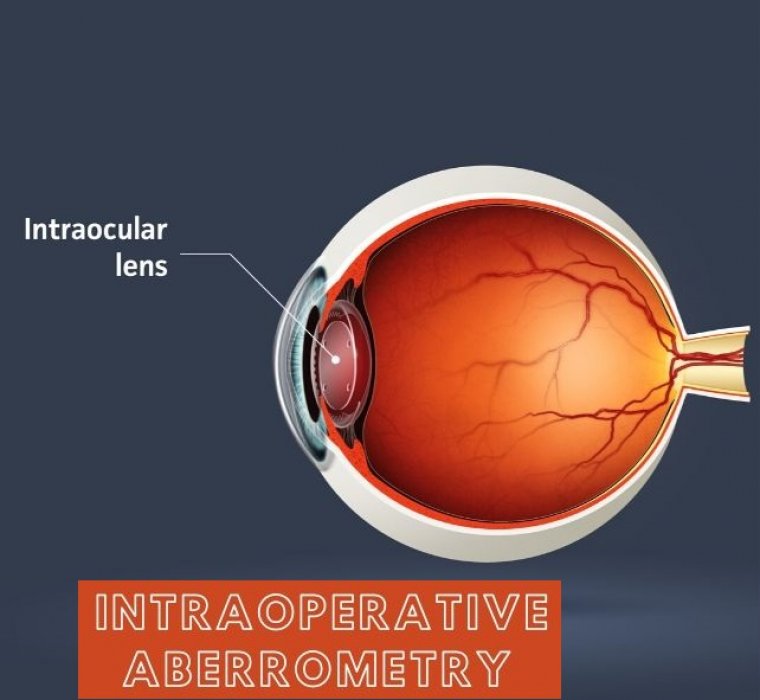
The effect of aging, namely cognitive impairment, decline in visual acuity and worsening motor function, may negatively affect surgical ability. However, age-related decline may be offset by the older surgeon’s years of clinical acumen, surgical experience and clinical judgement.
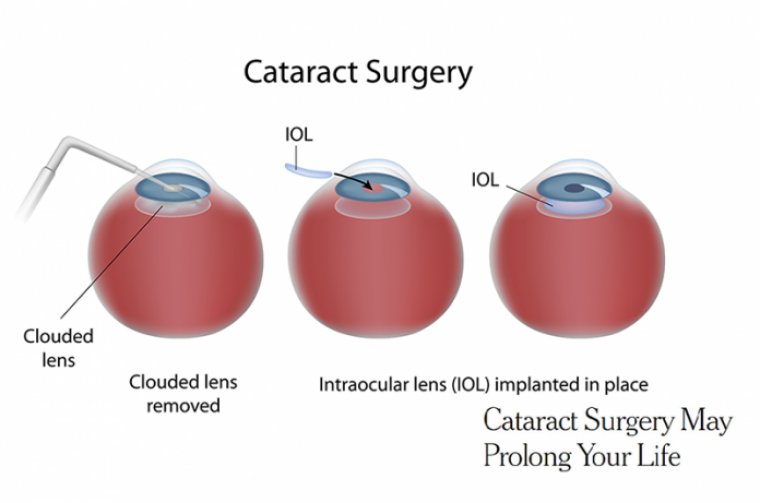
The old adage, “with age comes wisdom,” has been put to the test by a team at Queen’s University, Ontario, Canada. In an attempt to establish whether age increases the risk of adverse surgical outcomes, researchers studied almost half a million cataract operations between 2015 and 2020.
Of the 616,502 participants in the study, 39.7 percent of surgeons were 78 years or older.
“Late-career surgeons play a large role now in many areas of healthcare, including cataract surgery, which is the most common operation in most developed countries, and the average surgeon age is continuing to climb,” says Robert Campbell, Research Director at the university’s Department of Ophthalmology.
“At the same time, the overall population is continuing to age in most developed countries, creating a demand for healthcare that can’t be met by younger surgeons alone. As a result, we’re reliant on late career surgeons to provide a large portion of surgical care, and understanding how that affects quality of care is very important.”
So how did they fare? Well – really well. “Our study suggests that surgeons operating at later career stages provide high-quality, low-complication cataract surgery,” says Campbell.
Later-career surgeons performed a substantial proportion of cataract operations – one third of the overall patient sample – with surgical complication rates similar to those of midcareer surgeons.
“This likely stems from a few factors including that surgeons are staying up to date with technical innovations in the field and also that older surgeons are retiring at appropriate stages, before issues arise.”
Of the four individual complications, the only increase in risk concerned dropped lens fragment (0.11 percent) and suspected endophthalmitis (0.045 percent). “It’s important to note that overall complication rates were not higher among late-career surgeons,” says Campbell.
“Additionally, the absolute risks of these two specific complications were very low among both groups of surgeons, and, as a result, the difference in risk between older and younger surgeons was actually very small.”
Campbell notes that, with all studies, there is a risk that associations occur just by chance – however…
“Alternatively, the findings cannot rule out the possibility that some late-career surgeons may be less equipped to deal with some of the surgical challenges that lead to these specific outcomes. We’ll have to await follow up studies to understand why this association exists.”