Cataract Surgery & Astigmatism
Astigmatism is a condition that prevents the eye from consistently focusing light in all directions. This highly common condition is induced by an abnormal curvature of the lens or the eye itself, resulting in more of a football shape instead of a baseball.
Astigmatism can affect your near and distance vision, often causing mild blurring or double vision. We are able to determine the amount of astigmatism affecting your vision during your cataract evaluation.
Astigmatism can be corrected during the advanced laser cataract procedure. Depending on the amount of astigmatism, surgeons use the laser to create small incisions on the eye to reshape it. These incisions can be made more precisely with a laser compared to a manual procedure.
Limbal Relaxing Incisions (LRI)
Limbal Relaxing Incisions (LRI) are another way to correct minor astigmatism during cataract surgery. The LRI is typically performed at the beginning of surgery prior to IOL implantation. In this procedure, arc-shaped incisions are made to the surrounding periphery of the cornea.
This technique is designed to gently reshape and flatten the curvature of the cornea into a more spherical shape, ultimately eliminating astigmatism.
Toric IOL
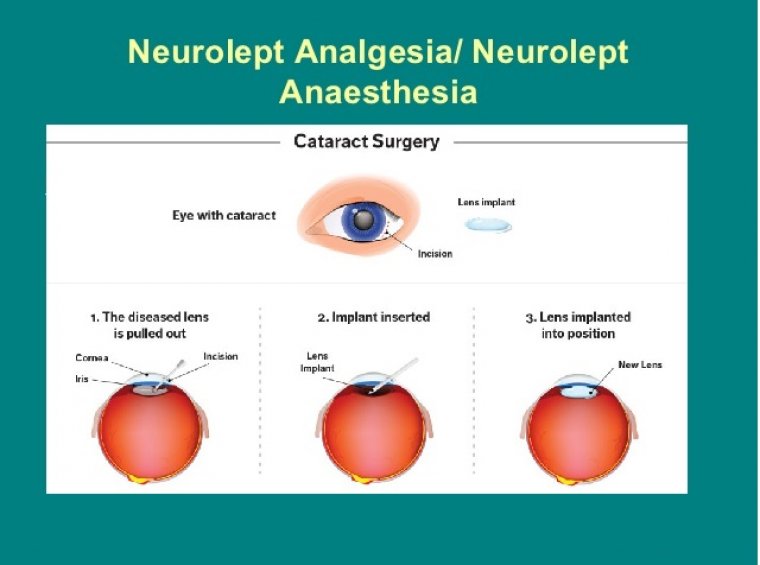
To treat astigmatism that is more severe, the cataract lens is replaced with a special intraocular lens (IOL), called a toric IOL. These lenses correct astigmatism as well as nearsightedness or farsightedness.
Like toric soft contact lenses, toric IOLs can correct astigmatism because they have different powers in different meridians of the lens. Because of how a toric IOL works, it must be properly aligned in the eye to provide the best visual outcome.
Astigmatism is very common in patients scheduled for cataract surgery. Although there are many devices that can measure astigmatism, they are not always in agreement. This presents a challenge when surgeons are trying to determine exactly how to treat patients with astigmatism.
The Cassini is in general the primary device for determining astigmatism power in axis in potential cataract surgery patients. It provides good accuracy for measuring the contribution from the front and back surfaces of the cornea.
Many surgeons use additional devices to confirm the astigmatism measurements, including the Pentacam and either the Argos Swept-Source OCT Biometer (Alcon) or the IOLMaster 700 Swept-Source OCT (Zeiss).
Of note, the IOLMaster 700 also provides both front and back surface measurements of corneal astigmatism. Once the total corneal astigmatism has been determined, the next challenge is marking the astigmatism axis on the eye on the day of surgery.
Automated systems, including the Callisto (Zeiss), Verion (Alcon) and ORA (Alcon), can help to make it easier.
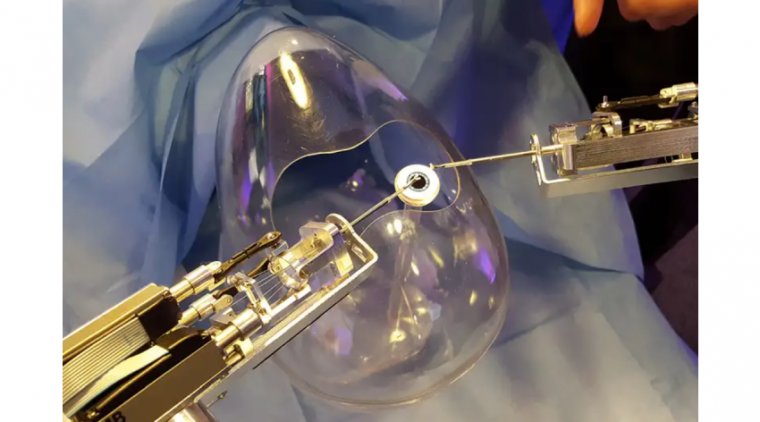
During the laser procedure, the laser uses the preop Cassini images of the iris to perform iris registration, which ensures proper alignment of the astigmatism marks. The laser then creates two nubs on the capsule on axis to provide a precise target for aligning the toric IOL intraoperatively.
The laser also creates two marks on the cornea on axis to further assist with alignment. Once the intraoperative portion of cataract surgery has started, there is very little additional time needed in toric IOL cases compared to standard IOL cases, as the capsular marks are in place.
The surgeon just has to align the marks on the toric IOL to the capsular marks. While intraoperative alignment technologies are effective options for optimizing alignment of toric IOLs during surgery, the final axis is not visible once the patient leaves the OR.
If the toric IOL ends up off axis by 10-15 degrees (for example), it is impossible to know if this is due to improper alignment intraoperatively or the toric IOL rotating.
With the presence of capsular nubs by the Lensar laser, the alignment of the toric IOL can be checked at any postop visit where the pupil is dilated to confirm that the toric IOL has remained on the same axis.
If the toric were to rotate, the surgeon can easily go back into surgery and reposition the IOL to the marks.
Along with the Cassini as a preoperative technology for evaluating astigmatism in patients scheduled for cataract surgery, having the Pentacam or a placido-based topography is important to identify irregular astigmatism.
Combined topography/wavefront systems such as the OPD-3 and iTrace are also effective technologies for surgeons who place toric IOLs, as they can provide an analysis on the toric IOL power and axis postoperatively.
If an adjustment to the toric IOL axis is needed postoperatively, the OPD-3 and iTrace can help with planning the direction and amount of rotation needed.
In summary, there are many preop and intraoperative technologies that can assist with the placement of toric IOLs.
As technology has advanced, surgeons can feel more confident that they can successfully treat astigmatism during cataract surgery.