Refractive Cataract Surgery - Patient Needs & IOL Performance
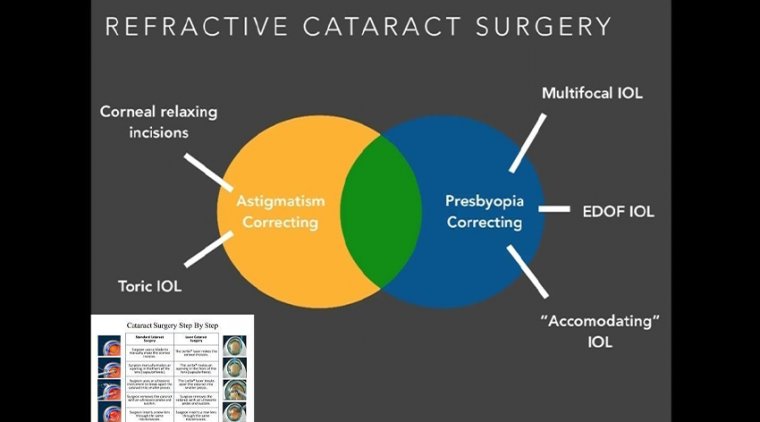
Modern multifocal IOLs can be considered as a surgical treatment not only for cataract but also for refractive purposes when implanted after clear lens extraction.
These lenses can be used to correct presbyopia, hyperopia, myopia, and, with toric multifocal models, astigmatism.
The primary aim of multifocal IOL implantation is to restore visual function and provide spectacle independence with a good level of patient satisfaction.
With proper IOL selection and successful surgical technique, spectacle independence can be expected not only at distance but also at intermediate and near.
In sports and other recreational activities, spectacle independence is desirable and can greatly improve a patient’s quality of life.
Most patients expect good visual outcomes after surgery, and most modern multifocal IOLs can deliver good near, intermediate, and distance vision.
This is an improvement compared with previous generations of bifocal IOLs, with which intermediate vision was frequently compromised.
Now with trifocal IOL technology, the addition of the intermediate focus has expanded the indication for this type of surgery to younger patients with a clear but dysfunctional crystalline lens.
PATIENT SATISFACTION
Obtaining a good surgical result and patient satisfaction depends on careful preoperative planning and individualized IOL selection based on the patient’s preexisting conditions, visual needs, and realistic expectations.
It also depends on the surgeon’s knowledge of the optical designs and visual performance of the available multifocal IOLs, proper surgical technique, and a comprehensive strategy for complications management.
The main reasons for patient dissatisfaction following multifocal IOL implantation are dry eye, residual refractive error (mainly astigmatism), and night vision complaints such as glare and halos.
Patient satisfaction after refractive cataract surgery depends on choosing an IOL that meets the individual’s needs for uncorrected vision but also tolerance to dysphotopsias.
According to Florian A. Kretz, MD, FEBO, approaches using rotationally asymmetric IOLs that do not have a diffractive optic design allow success for patients who are not willing to accept problems with glare and halos.
Dr. Kretz is medical director of Augentagesklinik Rheine and Greven, Germany. He discussed approaches using the Lentis-313 MF15 or MF20 IOLs (both from Oculentis) and the performance of these extended depth of focus implants.
“Choosing these approaches can result in very satisfied patients because the rotationally asymmetric IOLs provide high-quality vision and produce lower levels of dysphotopsias compared with diffractive presbyopia-correcting IOLs,” said Dr. Kretz.
MATCHING GOALS AND TECHNOLOGY
Dr. Kretz noted that cataract surgery patients interested in presbyopia correction can be grouped into three general categories based on their priorities forgood uncorrected vision postoperatively.
Some patients are near focused and have demands for excellent vision at reading distance (≤40 cm). Others seek good vision at all distances.
The third group is described as distancefocused patients most interested in clear vision at the intermediate to far range, and are willing to wear glasses for reading.
The strategies for addressing these visual needs include binocular implantation of the Lentis-313 MF15 or MF20 IOL with a refractive target of emmetropia.
These extended depth of focus IOLs provide a high degree of spectacle independence from distance to intermediate but also some functional reading vision. “These IOLs are aberration neutral,” Dr. Kretz said.
“Patients will use the spherical aberration of the cornea to enhance the depth of focus, which can improve their near vision.”
For patients with stronger near vision needs, surgeons can create blended vision using a micromonovision approach, implanting either the Lentis-313 MF15 or MF20 IOL bilaterally but targeting -1.25 D to -1.75 D in the non-dominant eye.
Another solution for providing good reading ability is to implant the Lentis-313 MF15 or M20 in the distance dominant eye and a multifocal IOL (Lentis MF30 or Mplus X) in the fellow eye.
Combining a pinhole lens (IC-8, Acufocus) in the near eye with the Lentis-313 MF15 of MF20 in the dominant eye can be a particularly good choice in patients who have irregular astigmatism. “
The pinhole hole can compensate for irregular astigmatism and is also not likely to cause dysphotopsias,” Dr. Kretz said.
CLINICAL PERFORMANCE
Outcomes data from testing of visual acuity, optical quality, defocus curves, and dysphotopsias provide evidence about the excellent clinical performance of the Lentis-313 MF15 and MF20 IOLs.
Dr. Kretz reported visual acuity results showing that the Lentis-313 MF15 IOL delivers distance visual acuity that is comparable to a monofocal aberration neutral IOL (CT Asphina 409).
Objective testing of optical quality (HD Analyzer, Visiometrics) also showed similarity between the presbyopia-correcting IOL and the monofocal lens.
Defocus curves from testing of patients implanted with some of the different approaches described by Dr. Kretz showed the wide range of good uncorrected vision achieved.
Testing for dysphotopsias conducted using a halo and glare simulator showed no difference in the occurrence or severity of these dysphotopsias comparing patients implanted with the EDOF IOLs versus the monofocal lens.
“Remember that even patients with a monofocal IOL can have halo and glare because of the presence of spherical aberration and other higher-order aberrations in the cornea,” Dr. Kretz said.
“If you look preoperatively at patients who have cataracts, you will see that their problems with dysphotopsias are even worse before surgery."