Management of the Dislocated Lens With New Techniques
In present times, cataract surgery has improved to such an extent that complications rarely occur. However, even after successful implantation of the intraocular lens (IOL), we may encounter IOL decentration or dislocation in some patients.
The decentration can occur either early or late. Early decentration occurs due to improperly made capsulorrhexsis and late decentration is seen following fibrosis of the capsule. Usual causes of decentration are improper fixation of the IOL, psuedoexfoliation, and post YAG capsulotomy.
A thorough history and examination must be done before planning the line of management. The condition could be managed by either medical or surgical means.
If the decentration is mild or symptoms occur during dilatation of pupil at night, it can be medically managed by instilling Pilocarpine eye drops. Surgical management of these cases depends on the type of implanted IOL and its location.
The decentred IOL can be either rigid or foldable. Rigid and three-piece foldable IOL can be easily placed in the sulcus, but single-piece foldable IOL cannot be placed in the sulcus and needs a different strategy.
In case the IOL is dislocated into the vitreous, the services of the vitreoretinal surgeon may be required.
Dislocated lenses, including both crystalline lenses and intraocular lens (IOL) implants, often occur due to weakened or damaged capsular support. They can occur as a result of intraocular surgical complications, ophthalmic trauma, or inherent zonular weakness from intrinsic causes.
These cases can be challenging to manage surgically, regarding both lens extraction or rescue and concurrent or subsequent implantation of a secondary IOL.
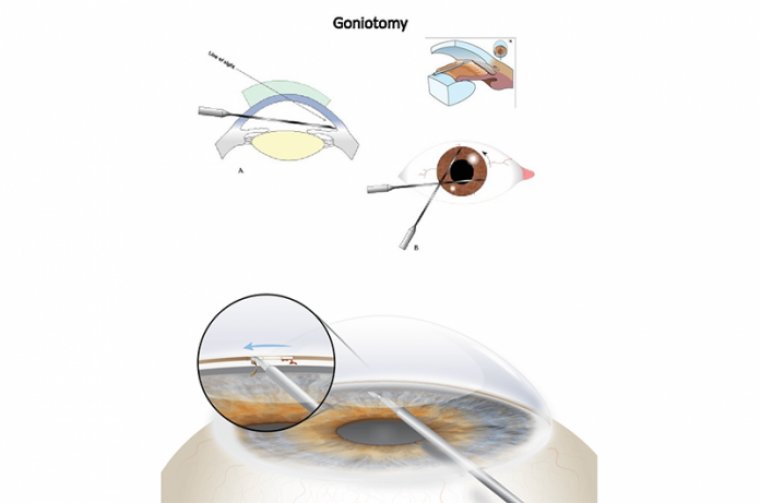
Although surgical options had previously been limited to anteriorchamber IOL implantation, multiple techniques for posterior implantation have since been described, including iris fixation, scleral suture fixation, and scleral sutureless fixation.
Future studies, however, will help better understand the long-term safety profile of these surgical approaches and how to minimize associated complications.
EVALUATING A DISLOCATED LENS
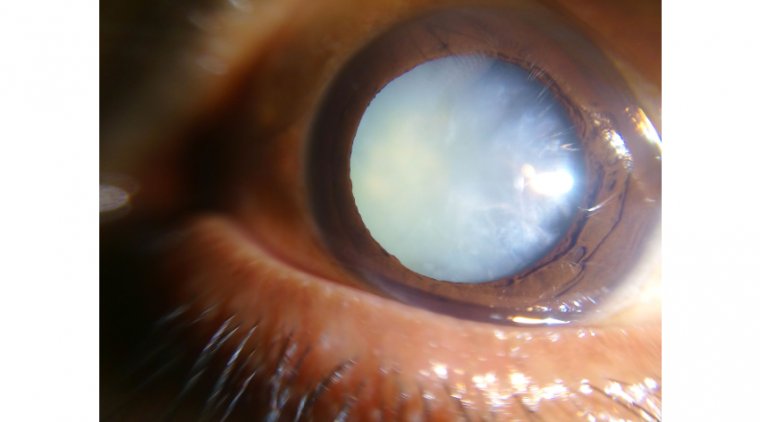
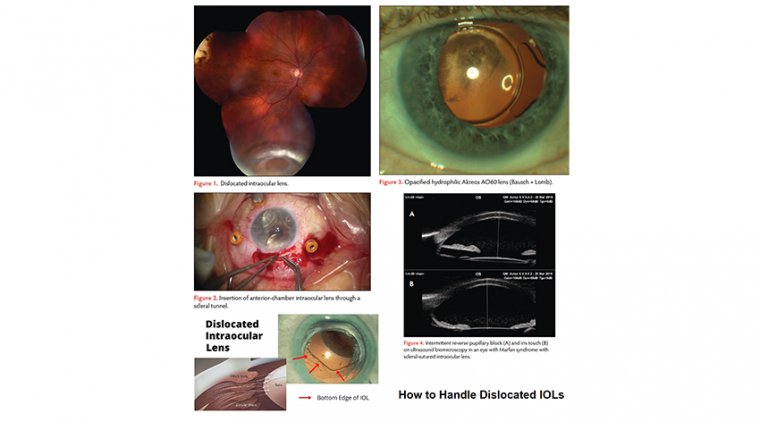
Dislocated lenses (Figure 1) are typically caused by insufficient capsule-zonular support. Risk factors include pseudoexfoliation, prior retinal surgery, prior ophthalmic trauma, high myopia, or the presence of a hypermature cataract, retinitis pigmentosa, diabetes mellitus, and history of acute angle-closure attack.
Associated systemic predisposing conditions may also be present, including Marfan syndrome, homocystinuria, hyperlysinemia, scleroderma, Weill-Marchesani syndrome, ectopia lentis et pupillae, and Ehlers-Danlos syndrome.
In general, symptoms of a dislocated lens can include decreased vision, monocular diplopia, pain, headache, and even sometimes seeing the edge of a lens implant. When evaluating an eye with a dislocated lens, assessment of certain findings may help in surgical planning.
Where is the lens or IOL located? What type of IOL is present? What is the IOL made of? What is the status of the vitreous?
Is there vitreous in the anterior chamber? Are other concurrent complications present: pupillary block, uveitis, glaucoma, corneal edema, vitreous hemorrhage, retinal breaks, or amblyopia?
In terms of workup, consider performing B-scan ultrasonography, especially if the posterior view is impaired, or ultrasound biomicroscopy to better evaluate the lens position.
Also, IOL measurements are useful for determining the power of an IOL implant. Finally, consider if associated systemic conditions need further evaluation.
TREATMENT OPTIONS
The surgical risk profile should be considered when weighing the approach to offer to a specific patient. If the lens is dislocated outside of the visual axis, nonsurgical management with aphakic correction could be considered.
This could be a preferable option in pediatric patients or in those for whom vitreoretinal surgery would have an increased risk of complications, like patients with Marfan syndrome.
If an aphakic contact lens is not a feasible alternative, there are many surgical approaches available for the management of dislocated lenses and subsequent refractive correction.
If surgical removal of the dislocated lens or IOL is necessary in combination with a vitrectomy, there are multiple options for secondary IOL placement. A commonly preferred option is to place an IOL “in the bag,” whereas the next option is a sulcus IOL.
If there is insufficient sulcus or capsular support, there are multiple options for a secondary IOL. These include anterior-chamber IOL (ACIOL), iris-sutured IOL, iris-claw IOL, scleral-sutured IOL, and scleral-fixated sutureless IOL.
In general, the technique that a surgeon is most comfortable with is often best for the patient. A recent meta-analysis by the American Academy of Ophthalmology found that there was “no superiority of any single IOL implantation technique in the absence of zonular support.”
That being said, certain factors can be considered when selecting a secondary IOL approach. Having more surgical options that you feel comfortable performing allows you the ability to adapt to different clinical scenarios.
ANTERIOR-CHAMBER INTRAOCULAR LENS
If there is not enough capsule-zonular support for a secondary sulcus IOL, one could consider an ACIOL. Traditional closed-loop ACIOLs have been associated with a high incidence of pseudophakic bullous keratopathy, pigment dispersion, and chronic iritis.
However, newer-generation open-loop ACIOLs have decreased contact with ocular tissues, leading to lower haptic erosion into the angle, thus causing less damage to the corneal endothelium.
Finn et al published a series of 50 eyes with secondary ACIOL placement with concurrent vitrectomy and found that few had long-term complications as there were no instances of persistent hyphema, vitreous hemorrhage, retinal break, retinal detachment, or IOL dislocation.
In a case series of 63 eyes, Khan et al found that combined vitrectomy with either an ACIOL or Gore-Tex (W.L. Gore) scleral-sutured IOL had similar visual outcomes. The relative ease of inserting an ACIOL compared with scleral-fixated IOLs make it an attractive option.
These lenses are often easily accessible and widely available and do not require mobilization of the conjunctiva, except to create a scleral tunnel (Figure 2). Drawbacks to ACIOL use include that it requires a larger corneal or corneoscleral wound and the IOL needs to be properly sized and placed.
To aid in insertion, it is important to properly size the scleral tunnel and achieve good hemostasis. A Sheets glide and acetylcholine chloride (Miochol-E; Bausch + Lomb) can be used to hold back the iris while inserting the IOL as well. The vitrector or Vannas scissors can be used to make the peripheral iridotomy.
IRIS-CLAW AND IRIS-SUTURED INTRAOCULAR LENS
Sutureless iris-claw lenses are fixated by a small knuckle of iris tissues on either side of the iris. They can be used with an anterior or retropupillary implantation and are most commonly used as phakic IOLs.
Iris-sutured IOLs involve directly suturing an IOL to the iris with one of several strategies, including the McCannel suture, Seipser knot, and girth-hitch knot. Potential complications of iris fixation including suture breakage, pupil ovalization, pseudophacodonesis and trembling vision, cystoid macular edema, pupillary distortion, synechia, pigment dispersion, and chronic iritis.
SCLERAL-SUTURED INTRAOCULAR LENS
A scleral-sutured IOL is a widely used option in refractive rehabilitation following removal of a dislocated lens. This can be used in eyes that have abnormal anterior-segment structures or insufficient capsular support.
Prolene suture was previously used, but this has fallen out of favor due to higher risk of breakage (approximately 28%). Expandable polytetrafluoroethylene (Gore-Tex) suture, which is used in cardiac surgery, is more preferred.
The foldable Bausch + Lomb Akreos AO60 IOL is a popular option that offers 4-point fixation and excellent outcomes. Khan et al published a series of 84 eyes undergoing PPV and scleralsutured IOL using Gore-Tex.
The authors reported a low rate of vitreous hemorrhage, macular edema, and ocular hypertension with no cases of endophthalmitis, suture erosion/breakage, or retinal detachment.
Having a consistent and precise system for passing sutures to loop eyelets correctly and working around the nose by rotating the IOL axis can help improve outcomes.
SCLERAL-FIXATED SUTURELESS IOL
To avoid sutures and their complications, sutureless techniques have been described, including using cannulas to create sclerotomy tunnels through which the haptics of a 3-piece IOL are subsequently pulled though.
Popular versions include the Yamane and modified Yamane technique with the Zeiss CT Lucia lens. These techniques appear to decrease specific complications related to suture degradation, which may be useful for younger patients.
However, this technique requires a high level of technical skill and has a risk of tilt/dislocation, iris chafe, and haptic erosion/endophthalmitis, corneal edema, retinal detachment, and intraocular hemorrhage.
To ensure a good outcome, it is important to achieve scleral fixation 180° apart, with 27-gauge cannulas at a similar angle to minimize tilt, and flanging with 27-gauge cannulas can help.
POTENTIAL COMPLICATIONS
Despite these advancements in secondary IOL placement, there are several specific complications to note. First, the Akreos AO60 lens is a hydrophilic 4-point fixation IOL that carries a small risk of opacification with air, gas, or silicone oil tamponade (Figure 3).
An alternative sutured IOL amenable to scleral suture fixation is the Bausch + Lomb Envista MX60, which is a hydrophobic lens that does not have a risk of opacification but has 3-point fixation instead of 4-point fixation.
Recent reports have suggested that there is a risk of breakage of the eyelets of this IOL. Additionally, suture erosion is a concern for both the scleral sutured and scleral fixated sutureless IOL as the overlying conjunctiva can erode and endophthalmitis can result.
Finally, reverse pupillary block is a risk (Figure 4), especially after insertion of scleral-sutured IOLs, even after a PPV. Although outpatient peripheral iridotomies can be useful, it is worthwhile to consider placing these prophylactically at the time of surgery.
There are multiple options for the management of dislocated lenses and the placement of secondary IOLs in the absence of adequate capsular support.
The technique that a surgeon is most comfortable with is often best for the patient, but learning new techniques and having the ability to adapt surgically can increase options. Further data are needed on the complications and long-term outcomes of these techniques.