The Role Of Premium IOLs & Posterior Corneal Elevation
Posterior corneal elevation very effectively discriminates keratoconus from normal corneas. Its efficacy is lower for subclinical keratoconus, and thus data concerning posterior elevation should not be used alone to stratify patients with this condition.
Corneal elevation topography is a sensitive method to identify patients who are potentially at high risk for developing ectasia after LASIK. The posterior corneal elevation map combined with corneal thickness values appear to be an important indicator of possible mild to suspect form of keratoconus.
It is widely accepted that patient selection is the key to success with premium IOLs. However, with care, premium IOLs can be implemented in challenging cases.
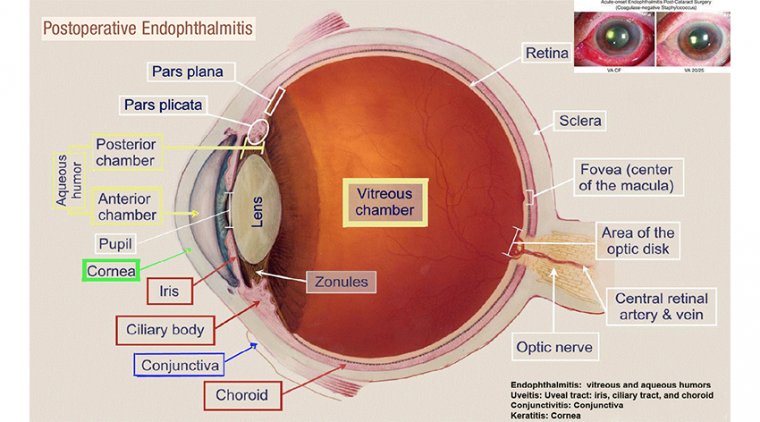
Premium IOLs have a very high-tech and sophisticated optical system that works excellently when the cornea is in perfect condition. Therefore, they are contraindicated in patients who have corneal haze, scar or oedema.
A patient who has a posterior corneal elevation is susceptible to higher-order aberrations (HOAs) or early keratoconus. Consequently, many surgeons will refrain from using premium IOLs in such cases.
Dry Climate & Keratoconus
In dry climates, keratoconus is prevalent due to the dry atmosphere, seasonal allergies and consanguinity. However, not all patients have the same severity of disease.
Some patients live their entire lives without knowing that they have keratoconus or without signs of the condition. Others present early with signs and symptoms.
Diagnosing Keratoconus
During diagnosis, all patients undergo a routine, complete ophthalmic examination, which includes dry and wet refraction.
Patients also undergo a meticulous clinical assessment and detailed history-taking, including family history, previous trauma, allergies, any spectacles changes and the frequency of these changes, and contact lens use.
Next, doctors perform corneal tomography, which is key for diagnosing keratoconus and precisely shows the anterior corneal curvature and the posterior corneal curvature.
Using four-maps analysis, doctors perform the Belin Ambrosio Enhanced Ectasia analysis and they study them carefully. Then they check the elevation maps, both in the forms of best-fit sphere and the best-fit toric ellipsoid.
They compare the maps and see if the patient has good spectacle correction. If the patient does not have high central aberration, then they consider implanting a trifocal lens.
Doctors speak with the patients about HOA photic phenomena and explain that they should anticipate some glare and halos over time. They even show them a picture of what glare and halo will look like so that they know what to expect in the coming weeks.
They also discuss mental adaptation and how their vision might be adapted to some aberration. The good thing about keratoconus patients is that they are already used to a minimum amount of light, glare and halos.
If their central vision is okay, it is not exaggerated by premium lenses. Almost in all cases, glare and halos turn out to be benign; however, doctors still like to set realistic expectations.
After performing a routine phacoemulsification and painstakingly centring the IOL, the plate haptic design IOL centres itself easily and this is a strong point in favour of this design.
Doctors like to place one suture to be sure that the lens does not move, especially if ectatic corneas have delayed healing or might have microleaks and fluctuation in eye pressure, which can change the lens position. If the patient is receiving a toric lens, it is ensured that the anterior chamber maintains its stability.
The postoperative regimen is similar to that of a routine phaco procedure. Doctors examine the patient and remove the suture within the first week and no later than 2 weeks from surgery. Then they reassess the patient’s vision at 2 weeks, 6 weeks and 3 months.
One step of utmost importance is assuring the patient that the lens is removable if he or she is not happy. Ophthalmologists offer patients a lens removal within the first 6 weeks if the aberration is higher than anticipated, and this provides some reassurance for the patient.
Case Studies
A 56-year-old breast cancer survivor with subclinical keratoconus wanted to treat herself after surviving her cancer by getting her eyesight back. She had heard about premium lenses and presented to us with a specific interest in trying them.
Considering her condition, we conducted an examination and determined that she was fine to move forward with the procedure. She told us that she was reborn after two things: recovering from breast cancer and being spectacle-free for the first time in her life.
A 48-year-old man in a sensitive diplomatic position presented to us and shared that his use of spectacles was causing some embarrassment because there are times when he was unable to wear them but still required to read things and he felt that this was disabling him. He was considering leaving his job due to his inability to focus.
He had posterior corneal elevation. The procedure was successful, and he has returned to work without anyone knowing that he had undergone the procedure.
Conclusion
Sometimes, surgeons can be afraid of technology because we do not know what is hidden behind it, and we refrain from exploring new advancements because we do not want our patients to have an unsatisfactory experience.
Given our recent experience with implanting premium lenses in challenging cases, we have changed our perspective and now view these opportunities as another way to give our patients a chance. In the end, the keratoconus patients who have received premium lenses are the happiest patients we have. This is probably because they are used to some amount of HOA so they adapt to their new IOLs faster and have higher tolerance than people with normal eyes.