How To Manage Iris Prolapse During Cataract Surgery
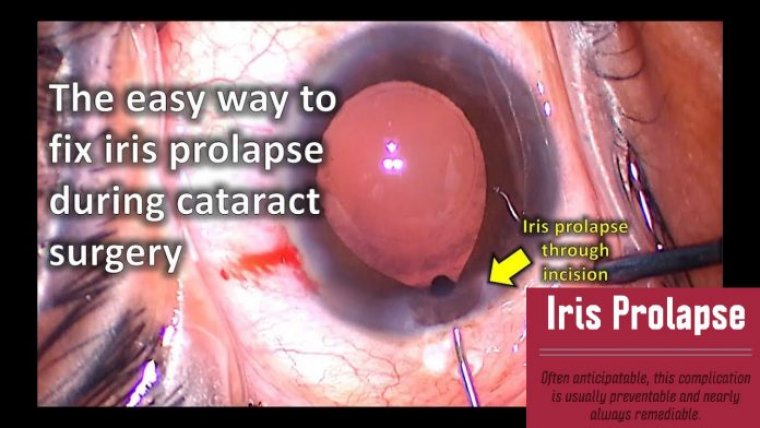
Iris prolapse is not an uncommon occurrence during cataract surgery. It usually occurs through the main incision during hydrodissection and is commonly associated with floppy-iris syndrome; however, it can manifest in cases with no known predisposition and can occur at any stage during surgery.
The mechanism is explained by the Bernoulli principle and its effect on iris position during the movement of fluid within the eye. Predisposing factors are iris configuration, anterior chamber depth, and position and architecture of the corneal tunnel.
Strategies for prevention and management include the use of pharmacological agents, ophthalmic viscosurgical devices, and iris retractors. These strategies can be augmented by alteration and adaptation of the surgeon’s technique.
We’ ve all been there before: the delicate iris prolapses out of our phaco incision during cataract surgery, making everything more difficult. Why does this happen? And how can iris prolapse be effectively managed?
Risk Factors for Iris Prolapse
An iris that does not have normal tone or anatomy may be more prone to prolapse during surgery. The iris is a kinetic structure with a complex of muscle fibers that allow it to adapt to light and focusing needs in a fraction of a second.
Many disease states can affect the iris and its ability to maintain muscular tone and adaptability, such as diabetes, hypertension, vascular diseases, anterior uveitis/iritis, syphilis, neurological disease, trauma and other factors such as certain systemic drugs.
Intraoperative Floppy Iris Syndrome (IFIS) has been described by David Chang M.D., in patients who have been taking tamsulosin (Flomax, Boehringer-Ingelheim). Tamsulosin is an alpha-adrenergic blocker primarily used in patients with prostate problems and difficulty with
urination.
Tamsulosin relaxes the muscles in the prostate and neck of the bladder in order to facilitate good urine flow. The use of tamsulosin and similar drugs is increasingly common due to the natural aging process and hyperplasia of the prostate.
Unfortunately, tamsulosin may also cause excessive relaxation of the iris muscles and may contribute to the iris having a very low tone a floppy iris.
During cataract surgery, a floppy iris is likely to prolapse out of the corneal incisions due to the pressure variations created by phacoemulsification.
Cataract incisions can also play an important role in iris prolapse. Clear corneal incisions that are too posterior, situated too close to the iris root, may contribute to issues of prolapse.
In addition, excessively leaky incisions are a significant contributor as creation of large currents of fluid flow will likely cause the iris to billow out of the eye as well.
Eyes where the papillary dilation is weak are also more prone to iris prolapse because there is more iris tissue accessible to the incisions.
Extraocular forces can also contribute to iris prolapse, such as the case with an overly voluminous retrobulbar injector or a forceful lid speculum. These can both cause posterior pressure on the globe, thereby increasing the pressure behind the cataract.
When incisions are made in the anterior chamber, dropping the anterior chamber pressure dramatically, this posterior pressure creates a gradient.
Pressure Gradients are Key
All cases of iris prolapse can be explained with the concept of a pressure gradient. The iris will tend to move from the area of high pressure to the area of low pressure.
This mismatched pressure gradient causes the iris to prolapse. Therefore, the best way to correct the problem is to equalize the pressure gradient.
Causes of high pressure behind the iris include:
Intraocular causes
– capsule block syndrome during hydrodissection
– broken posterior capsule with hydrated vitreous during hydrodissection
– trapped viscoelastic or saline behind the iris
– choroidal hemorrhage
– relative high vitreous pressure in nanophthalmic eyes
Extraocular causes
– excessive retrobulbar anesthetic injection
– tight lid speculum
– patient squeezing/valsalva maneuver
The iris does not naturally prolapse out of the eye, but when the pressure gradient is such that the posterior pressure is much higher than the anterior pressure, the iris is forced to flow out of the incision.
The techniques that we have been taught to rectify this problem are all methods to equalize the pressure
At the end of the case, with no viscoelastic in the eye, the iris may tend to prolapse again due to the pressure gradient. By lowering the pressure behind the iris, the pressure gradient can be equalized and the iris will return to the eye.
For extreme cases, giving the patient intravenous mannitol or even performing a partial pars plana anterior vitrectomy to decrease the posterior pressure may be appropriate options.
However, for most cases of iris prolapse, simple techniques can be employed to restore the iris to its anatomic position and successfully complete the cataract surgery.
Managing Iris Prolapse: Nucleus Removal
During nucleus removal via the phaco probe, it is common to have the inflow irrigation flow behind the iris, which further contributes to the pressure gradient and the iris prolapse.
In this situation, it is easier to increase the pressure in front of the iris to equalize the pressure gradient.
This can be achieved by placing a plug of a super-cohesive viscoelastic on top of the subincisional iris. Here, a traditional cohesive viscoelastic would work, however a viscoelastic such as Healon 5 (Advanced Medical Optics [AMO], Santa Ana, Calif.) is a better choice.
Currently, Healon 5 and Healon GV (AMO) are the only viscoelastics in the category of super-cohesive or visco-adaptive.
Steps After Viscoelastic Removal
The Healon 5 plug can be used effectively during most of the surgery: apply a plug during phaco, apply another plug during cortex removal, then apply a final plug before IOL insertion.
However, at the end of the case, when the IOL is safely within the capsular bag and we want to remove the viscoelastic, how do we solve the iris prolapse?
In this situation, there is fluid behind the iris, causing it to billow and prolapse outside of the eye. The first step is to use the Osher technique of hydrating the clear corneal incision prior to removing the viscoelastic.
After removal of the viscoelastic, the iris will tend to prolapse. At this point, use the cannula or a second instrument to flatten the anterior chamber and release the fluid that is trapped behind the nucleus.
Now, with a flat anterior chamber, there should be no pressure gradient and the iris should automatically return to its normal position within the eye. Use balanced salt solution on a cannula to re-inflate the anterior chamber via the paracentesis.
As you re-inflate the anterior chamber, you can direct your stream of balanced salt solution on top of the iris to prevent prolapse.
In summary, the management of iris prolapse involves equalizing the pressure gradient. Determine the cause of the increased posterior pressure and then either increase the pressure in front of the iris by applying a plug of Healon 5 or decrease the pressure behind the iris by releasing trapped fluid. Once the pressures are equalized, the iris will naturally return to its normal position.