Diagnosing Irregularities In The Corneal Surface Before Cataract Surgery
Better comfort, better high-contrast sensitivity (eg, Snellen chart) and quality of vision (less shadow vision, glare, or halos), and less fluctuation of vision are among the reasons to treat corneal surface irregularities in all patients, even in those not contemplating cataract surgery.
However, treating these irregularities prior to cataract surgery is key in order to obtain more accurate measurements of the corneal curvature. Otherwise, it can lead to errors in IOL power selection and orientation of toric IOLs.
A thorough slit lamp exam and corneal topography are required before cataract surgery to diagnose irregularities in the corneal surface.
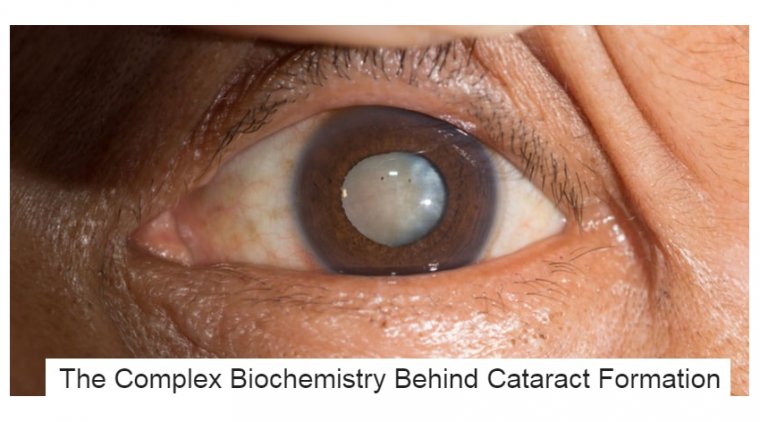
Many times, complex corneas of patients coming in for a cataract consultation are easy to spot. A scar or significant pathology can be quite obvious at the slit lamp.
Other complexities are more subtle, however, and can be easily missed without a thorough investigation — epithelial basement membrane dystrophy (EBMD) is one example.
Irregular astigmatism will not necessarily be observed on exam but will show up on topography. Surgeons should not assume that a complex cornea is a straightforward presentation, and they should always be on the lookout for these patients.
Affects timing, IOL calculations and technology
A complex cornea not only affects the timing of cataract surgery, it can also have an impact on the accuracy of IOL calculations as well as the lens selection — some patients will not be a candidate for the available premium technology.
It is important to note that pathology can also be the cause of a patient’s visual disturbance and not the cataract. Teasing these factors out is paramount for proper management of complex cornea patients.
Another consideration is the location of the corneal irregularity. In some cases, the cornea can be improved before cataract surgery, but in other situations, this is not possible.
When the irregularity is located closer to the surface of the corneas as in severe ocular surface disease, pretreatment can often allow the patient to enjoy excellent postoperative outcomes with premium technology.
Even EBMD with a centrally located irregularity can be improved by performing a superficial keratectomy, and Salzmann’s nodules too can be removed and the cornea subsequently “regularized.”
Higher-level irregularities of the entire corneal stroma such as keratoconus or deep corneal scars cannot be mitigated before a cataract procedure. In these cases, surgeons must consider the best outcome they can achieve for the patient with the cornea as it exists. Clearly this scenario will have a more drastic impact on the IOL choice and what can be expected for postoperative vision.
The two elements critical in the cataract workup to identify complex corneas are a detailed slit lamp exam and topography or corneal surface mapping.
A good slit lamp exam is important because subtle things can be missed on topography and vice versa. Both of these need to be considered together — they really go hand in hand.
A person can have what looks like obvious dry eye disease on topography, but on a slit lamp exam, it is discovered that EBMD is the cause of the irregularity.
One can perform a quick slit lamp exam and then see a hot blue spot on topography. Upon going back and lifting the lid, the patient can have a superior Salzmann’s nodule affecting central corneal regularity.
Can’t count on patients’ memories
It is fairly common for surgeons to encounter patients who are unaware that they have a condition that constitutes a complex cornea. Many do not recall having had previous surgery, for example.
This underscores the importance of performing corneal mapping as part of the cataract workup so as not to overlook any subtle corneal irregularities.
In each of our practices, we often see patients with a history of LASIK with an off-center treatment, yet these patients are unaware that this has implications for their cataract procedure.
In those situations, corneal irregularities will be magnified once the natural lens is removed. These patients may not be good candidates for a multifocal lens.
Other technologies that can be helpful include iTrace (Tracey Technologies) to identify higher-order aberrations, especially in post-refractive patients; tomography for elevation and higher-order aberration data; and pachymetry or anterior segment OCT for corneal thickness.
We both practice in tertiary care centers; therefore, we see an even higher percentage of complex corneas — as many as 25% or more — than what might be typical in a different type of practice, and ethnicity also plays a role in prevalence.
For example, Middle Eastern patients have a higher rate of keratoconus. Performing a detailed slit lamp exam and corneal topography is essential for identifying complexities of the cornea when evaluating cataract patients.