Cataract Surgery & Diabetes
Diabetes mellitus is a disease of elevated blood sugar due to insufficient production (type 1) or action (type 2) of insulin. Type 1 diabetes requires insulin injections, whereas type 2 is managed with diet, exercise, tablets or insulin injections, if needed.
Cataract surgery can influence the progression of diabetic eye disease, but may be necessary for treatment and to help the person function effectively.
The impact of cataract is twofold.
- Poor view of the retina means that laser and intravitreal injections to treat the visual complications of diabetes, such as diabetic retinopathy or maculopathy, might become impossible. Without treatment, these can progress to the point where potential vision is so poor that cataract removal will not lead to visual improvement.
- Failing sight, due to cataract, cause practical difficulties with the timely administration of medication to control blood glucose (blood sugar). This is especially true for those who have to inject insulin.
Unfortunately, cataract tends to have an early onset in those with diabetes and progresses rapidly if blood sugar control is suboptimal. This is most likely due to the osmotic changes taking place within the lens, usually resulting in cortical or posterior subcapsular lens opacities.
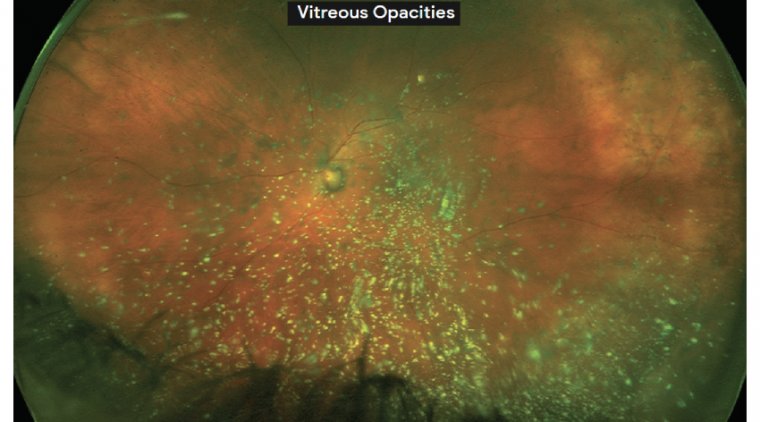
Some studies have reported that cataract surgery when performed in diabetic patients may lead to relatively rapid progression of DR, precipitate vitreous hemorrhage, induce iris neovascularization, and ultimately lead to decrease or loss of vision.
The safety and success of cataract surgery has improved so dramatically in recent years that it can sometimes be difficult to bear in mind the unique needs of special patient populations that might necessitate a change in surgical approach.
But the diabetic population in the US — 55 million strong and growing — are becoming an everyday occurrence in cataract surgery suites, and even the most highly skilled surgeon may have trouble fully grasping the consequences of diabetic eye disease.
Cataract is an important clinical problem affecting patients with diabetes mellitus. Both type 1 diabetes and type 2 diabetes are associated with an increased frequency of cataract surgery.
The Wisconsin Epidemiologic Study of Diabetic Retinopathy reported that the cumulative incidence of cataract surgery in patients with type 2 diabetes is about 25% over 10 years.
There is a complex relationship between diabetes mellitus and cataract progression. For example, the Beaver Dam Eye Study reported a statistically significant association between diabetes mellitus and cortical lens opacity.
On the other hand, a recent prospective study reported a negative association between ischemic diabetic retinopathy and progression of nuclear sclerosis.
Similarly, there is a cause-and-effect relationship between cataract formation and certain therapies used in the treatment of diabetic retinopathy. For example, clinical trials have documented that intravitreal triamcinolone acetonide is associated with cataract progression.
However, the relationship between pars plana vitrectomy and cataract progression is less certain, at least in diabetic patients.
There is a well documented association between PPV and cataract progression in non-diabetic patients, but several studies have found no association, or even a negative association, between PPV and cataract progression in diabetic patients.
Some studies have reported an association between cataract surgery and progression of diabetic retinopathy, but other studies have reported no significant association.
Further complicating our understanding is the fact that, in pseudophakic diabetic patients, it may be difficult to distinguish early diabetic macular edema from pseudophakic cystoid macular edema. Some diabetic patients may show features of both CME and DME following cataract surgery.
The Early Treatment Diabetic Retinopathy Study (ETDRS) published follow-up data on the subset of enrolled patients that subsequently underwent cataract surgery.
The ETDRS reported that, at one year following cataract surgery, visual acuity improved by two or more lines in 64% of eyes randomized to early photocoagulation and in 59% of eyes randomized to deferral of photocoagulation.
To better study these relationships, the Diabetic Retinopathy Clinical Research (DRCR) network is planning two trials. Protocol P is a non-randomized cohort study of patients with center-involved diabetic macular edema undergoing cataract surgery.
Protocol Q is an observational study of patients with diabetic retinopathy without center-involved DME undergoing cataract surgery.
Both studies are currently recruiting. With careful follow-up of these patients using standardized ETDRS visual acuity testing and optical coherence tomography, a better understanding of the association between cataract surgery and DME will be possible.
Considerations & Modifications
With these concepts in mind, certain recommendations become evident when faced with a patient with concomitant diabetic retinopathy and cataract.
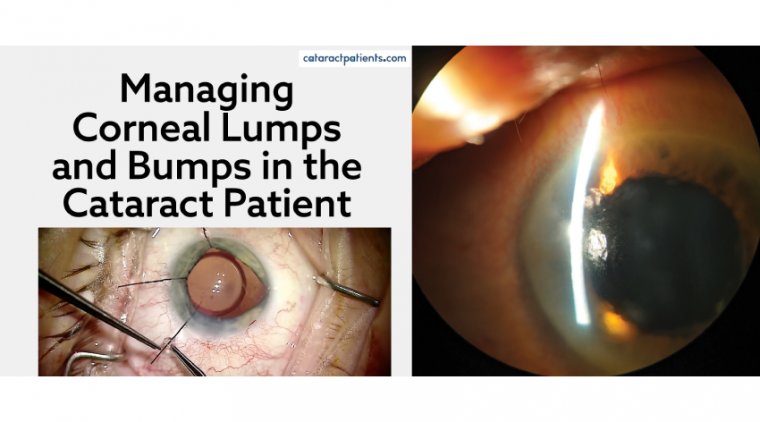
First, the determination of a visually significant cataract in a patient with pre-existing diabetic retinopathy may be more difficult than in a patient with a normal posterior segment.
Tests such as a potential acuity meter or potential acuity pinhole may be helpful in certain patients to determine what component of the visual loss is due to the cataract rather than the retinopathy.
In addition, optical coherence tomography is widely employed before cataract surgery to assess the potential for coexisting retinal disease to limit postoperative visual performance.
OCT may be particularly helpful in cases where visualization of the macula is hindered by dense lens opacity and in cases where the visual loss appears out of proportion to the degree of cataract.
Second, when possible, it appears prudent to treat preexisting diabetic retinopathy prior to scheduling elective cataract surgery.
This may appear obvious, but several caveats must be considered. Depending on the density of the cataract, it may be difficult to properly diagnose or treat retinopathy prior to cataract surgery. In addition, diabetic retinopathy may persist despite appropriate treatment.
For example, the DRCR has reported that at least 50% of patients with DME will have persistent edema two years following focal/grid photocoagulation.
In another series, 52% of eyes with persistent DME following focal/grid photocoagulation manifested definite signs of vitreomacular interface abnormalities, including anomalous vitreomacular adhesions, epiretinal membrane, or both.
Therefore, it may not be feasible to delay cataract surgery until the macular edema has completely resolved.
Third, certain modifications to the surgical strategy become important in patients with advanced diabetic retinopathy, or in patients judged likely to progress in the future.
For example, silicone intraocular lenses are associated with visually significant moisture condensation during fluidair exchange and may be a suboptimal choice in a patient deemed likely to require subsequent pars plana vitrectomy.
Additionally, presbyopia-correcting intraocular lenses may be problematic for many reasons in the diabetic population.
Patients with pre-existing macular diseases, such as DME, have impaired contrast sensitivity and may be particularly dissatisfied with their visual quality following implantation of a premium IOL, particularly a diffractive multifocal lens, owing to the light-splitting nature of the refractive correction provided.
Although spectral domain OCT has greatly improved our ability to evaluate the macula prior to cataract surgery, some eyes will have a guarded visual prognosis, and this should be explicitly discussed with the patient and family members during the informed consent process.
With these recommendations in mind, most diabetic patients will achieve favorable anatomic and visual outcomes following cataract surgery.