How to Manage Irregular Astigmatism in Cataract Surgery
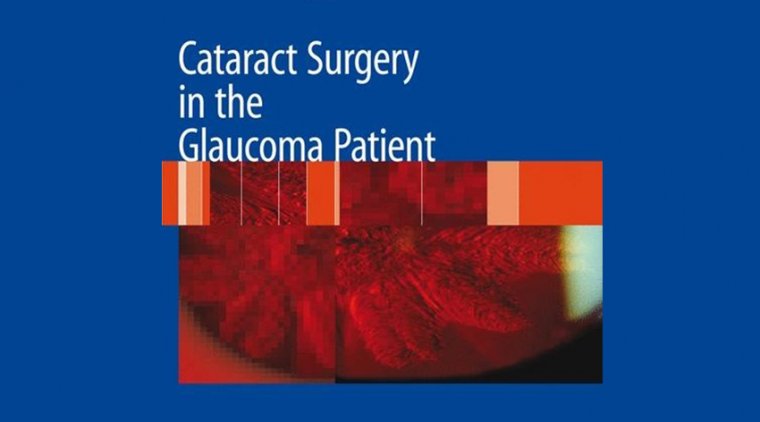
Toric lenses currently have the most predictable results, are the most cost-effective in the long term, can correct the highest amounts of astigmatism and are relatively easy to use.
This method of correcting astigmatism is well-studied and has become more reliable with current technologies and algorithms that allow for accurate, intraoperative measurements.
LRIs have less predictability and efficacy compared to toric lenses, but they can be used effectively in patients with lower levels of astigmatism.
Clear corneal incision placement on the steepest meridian is the least expensive option for patients with low levels of astigmatism. However, smaller phaco incisions have made this option less effective since only small amounts of astigmatism can be corrected.
Two-stage procedure with excimer laser ablation is a good option for treating residual astigmatism and spherical error post cataract surgery, however the cost can be prohibitive.
Astigmatism is a common eye condition that exists when the surface of the cornea or crystalline lens is irregularly shaped. It is a form of refractive error that can be present alone or in combination with myopia and hyperopia. Its correction requires the use of cylinder lens power.
The eye’s total refractive astigmatism is a combination of corneal and lenticular astigmatism. Most astigmatism comes from the cornea. The average lenticular astigmatism is 0.5 diopters against-the-rule (ATR).
The amount of lenticular astigmatism can be calculated by subtracting corneal astigmatism from the total astigmatism found by refraction. Since lenticular astigmatism is eliminated with extraction of the cataract only the corneal astigmatism is considered when planning cataract surgery.
There are several different approaches to handling regular and irregular astigmatism during cataract surgery, but still much debate on which solutions are most effective given unique patient circumstances.
When people talk about astigmatism and intraoperative aberrometry, the conversation is often made with the assumption that the cornea is normal and regular.
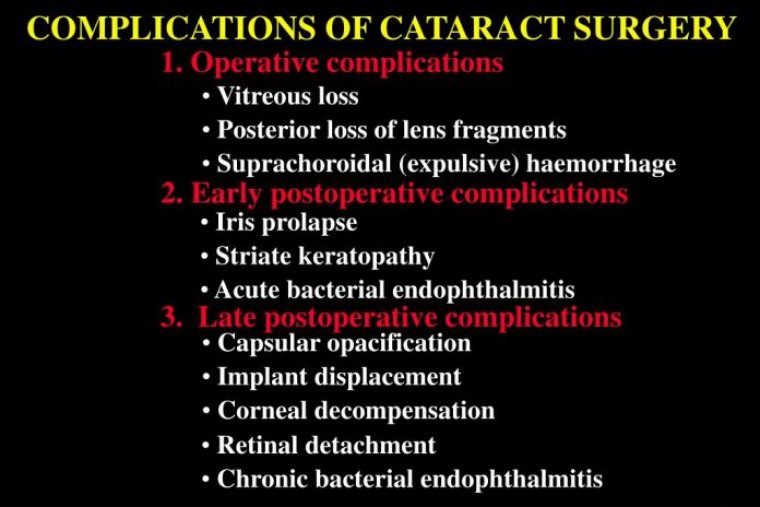
Irregular astigmatism in patients presenting for cataract surgery (or refractive lens exchange; RLE) can have consequences: poor vision. For the surgeon, this is partly because the biometry can be challenging, which makes accurate IOL calculations difficult. Any error results in a refractive miss, causing both the patient and surgeon grief.
To deal with irregular astigmatism, we first have to understand its cause.
Why Corneas Become Irregular
Let’s look at the cornea systematically from front to back. There are five layers and three of them are responsible for irregular astigmatism. The tear film sits atop the cornea, and needs to be regular in its consistency to provide regularity of the corneal surface.
The epithelium translates to the tear film and, if that is irregular then, once again, we have irregular astigmatism. You cannot forget the subepithelial area; there are conditions that affect this region and they also translate right across to the front surface of the cornea.
And then there is the stroma; if it is scarred, ectatic or abnormal in in terms of shape that may also cause irregular astigmatism.
Dry Eye
Dry eye is probably the single biggest cause of irregular astigmatism. It’s something that cannot be dismissed – and, in this age of refractive lens exchange and refractive cataract surgery, we are appropriately giving this topic a great deal of attention.
We all know the causes of dry eye: underproductive, evaporative and inflammatory, but remember, an irregular tear film can exist in asymptomatic patients.
Tear osmolarity can be used as a measure of dry eye, and Epitropoulos et al. showed that patients with hyperosmolar tear film occasionally display great variation in terms of their keratometric cylinder plus, their IOL calculations varied by 0.5 D in 10 percent of cases. Dry eye really is not a trivial disorder, and it certainly does not have a trivial impact on IOL calculations.
Irregular Astigmatism Irising From The Sub-Epithelium
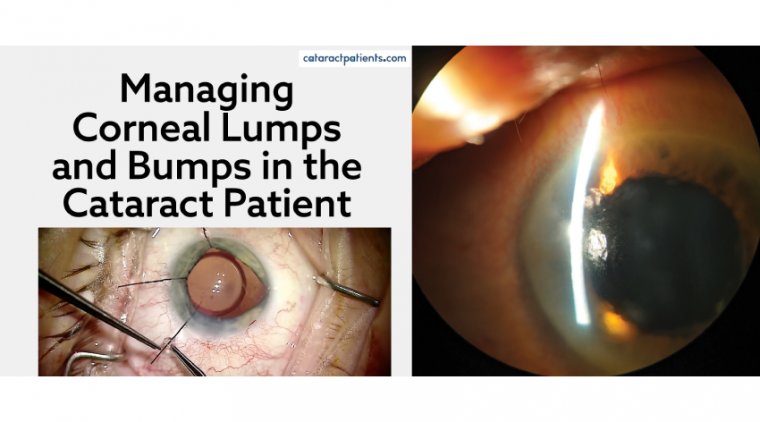
Salzmann’s nodular degeneration can also cause problems. Even if the degenerative nodule is peripheral, it can influence central keratometry and regularity.
You may be able to risk performing a cataract operation on this patient – but, if the nodules progress and eventually need removal, you have got a whole new keratometry to deal with; each case needs to be carefully considered.
Stromal Irregular Astigmatism
Both scarring and ectatic disorders can cause irregular corneal astigmatism from the stroma. Such patients are not easy to deal with.
Corneal shape changes can commonly cause irregular astigmatism. They often present as asymmetric bow ties; if they’re orthogonal, then they are on the correct axis, the cornea is just steeper inferiorly than above and that’s not bad, because the overall astigmatism is fine – it’s when they’re non-orthogonal that it’s a problem.
If you’re going to use a toric lens in a non-orthogonal astigmatic patient, then the biggest question is: where to orientate the implant?
Diagnostics of Irregular Astigmatism
We are doctors – and one of the most fundamental aspects of the profession is evaluating patents clinically.
A comprehensive clinical evaluation is vital in diagnosing irregular astigmatism, but we do also have a number of diagnostic instruments available to help us. And they can also be used to monitor disease progression (and improvement) of patients.
When we look at a patient, going from front to back; first, we look at the tear film, then look at the shape, clarity and surface of the cornea to see if there is anything that might influence things. Next comes a fluorescein stain to check lid action and the distribution of the fluorescein dye.
If patients are not closing their eyelids properly and have exposure, then they may need to be seen by an oculoplastic surgeon before proceeding to cataract surgery.
What tools do we have at our disposal, if we suspect there is a problem and want to know the magnitude of that problem?
First, you need a Placido-based reflective topographic system, and there are some great markers devised by Steve Klyce that can be used to flag irregular corneas: the Surface Regularity Index (SRI) is used a lot; the Standard Deviation of (corneal) Power is also a good one.
Some Placido systems are combined with aberrometry systems (such as the Nidek OPD 3, Tracey Technologies’ iTrace and Topcon’s KR1W).
They all work in slightly different ways, but all are excellent at providing truly useful information about the surface and overall aberrometry, and by subtracting corneal-derived aberrations from the overall aberrations, internal aberrations can be calculated.
Three-dimensional diagnostic instruments (for example, the Orbscan [B+L] with its scanning slit approach or the Scheimpflug-based systems: Oculus’ Pentacam, Ziemer’s Galilei or Visionix’s VX120 family) offer shape analysis – elevation, posterior cornea and corneal thickness, which is really useful information when it comes to dealing with the corneal shape.
Anterior segment OCT is now coming into vogue and I suspect will displace some of the current “gold standard” devices being used.
Management Strategies
The principles of management are simple: eliminate and reduce corneal irregularity by addressing the source of the problem by either medical therapy (for example, when the cause is dry eye) or surgical intervention.
Follow-up is important; the cornea needs to be evaluated to see how the patient’s eye is progressing. Has the surface got smoother; has the tear film improved? Has the surface stabilized?
If a patient presents with dry eye, evaluate the cause and treat it. Once the tear film is stable, biometry and IOL calculations can be performed with some confidence. The key is to proceed from stable foundations, rather than highly fluctuating ones. But what about the aforementioned corneal disorders?
Anterior Basement Membrane Dystrophy
Anterior basement membrane dystrophy results from a duplication of basement membrane, which causes an irregularity you can see on the fundus retroillumination picture.
Typically, epithelial debridement (even at the slit lamp) followed by a bandage contact lens is sufficient in such cases – occasionally we’ll add photo-therapeutic keratectomy (PTK) – 5–10 µm laser ablation in PTK mode – to promote good healing and adherence.
Non-Orthogonal Astigmatism
What causes non-orthogonal astigmatism? Ectatic disorders like keratoconus mostly, but it can also occur in post-corneal graft patients. So how does one deal with those patients who have got corneal ectasia or keratoconus?
We always try and find out from the optometrist what the BSCVA was before the cataract. If it was 6/12 or better I’d probably go ahead and do a lens calculation and put a toric lens in.
If it was less than 6/12, then we’d have to try and find a way to regularize the corneal shape either by use of intracorneal rings or corneal cross-linking (CXL) with topo-guided PRK. The last resort would be corneal transplantation.
The Bottom Line
As noted, the principles of managing irregular astigmatism cataract surgery are actually pretty simple: find the source of the problem, address it as best as you can, then only proceed to ocular biometry, IOL calculations, and surgery when the astigmatism is compatible with potentially good vision.
If we can follow those rules, then we do not need to fear irregular astigmatism in cataract surgery: we can embrace it instead!